Human Chorionic Gonadotropin (HCG)

HCG levels are important in determining the health of the fetus in early pregnancy. Higher or lower than expected levels at certain points during pregnancy can be associated with certain complications.
However, the common belief that HCG levels consistently double every 48 hours in early pregnancy is not correct. HCG levels can double every 1 to 5 days and still result in a viable pregnancy.
Researchers still have more to learn regarding HCG levels, as numerous factors can affect these values such as ethnicity, body mass index, smoking, sex of the fetus, number of fetuses, and placental weight. Two different women with viable pregnancies at the same gestational age can have dramatically different HCG levels.
Women should read below to better understand current research regarding the function of HCG during pregnancy and what HCG values may indicate during early pregnancy.
Background
Human chorionic gonadotropin (HCG) is a hormone produced by the trophoblasts of the developing placenta.
After implantation, the embryo actively secretes HCG, which can be detected in the mother’s blood as early as 8 days after ovulation. HCG lets the body know a pregnancy has occurred and the rest of the body begins changing to support it.
HCG is the longest circulating molecule in human blood and is made almost exclusively in the placenta, and is therefore made only during pregnancy.
One of the first functions of HCG is to help maintain the corpus luteum (CL) and its progesterone production, which is essential for successful implantation. If HCG is not secreted at implantation, the CL stops producing progesterone and mensuration begins.
HCG is also linked to umbilical cord development, suppression of uterine contractions, and the growth and development of fetal organs.
New research is finding HCG receptors in fetal organs such as the kidney, liver, spleen, and small and large intestines. It was previously unknown if HCG had any direct effect on the fetus itself, but now it is theorized that HCG may promote fetal growth. It is also possible the fetus produces its own HCG from the kidneys and liver, but more research is needed to determine the exact function of these receptors.
Interestingly, these receptors are present in fetal organs but are completely absent in adult organs. Therefore, it is currently assessed these receptors disappear at birth.

Levels (General)
HCG levels are reported in milli-international units of HCG hormone per milliliter of blood, or mIU/mL. International unit per liter (IU/L) may also be used.
Once the level of HCG in the blood crosses a certain level, it can be detected in the urine; this is when a urine pregnancy test shows a positive result.
Pregnancy tests typically start at 20 to 50 (reportedly as low as 6.3 to 12.5) mIU/mL. Blood tests can measure HCG as low as 1 to 2 mIU/mL. It is estimated that at the time of an expected period, a woman's HCG level should be around 100 mIU/mL.
A false negative, in which a woman is actually pregnant but the test showed a negative result, can occur if the test was taken too early, the urine was too diluted, or the amount of HCG in the blood is so high (500,000 mIU/mL) the test cannot work properly (known as a hook effect).
Levels of HCG in early pregnancy are important markers of embryo health. Abnormal levels of HCG have previously been associated with fetal loss, preeclampsia, preterm delivery, and fetal growth restriction.

However, normal values have not been determined and there is great variability between women at the same week of pregnancy. Wide variation also applies to the rate of rise, doubling, and peak. Further, very little is known about gestational time-dependent effects of HCG on potential negative outcomes of pregnancy.
At least one study showed that among women whose pregnancies resulted in normal term deliveries, HCG levels in the blood of those women at the end of 6 weeks of pregnancy were shown to vary from 440 to 142,230 mIU/mL.
Despite this variability, average ranges appear to be:
0 to 4 weeks of pregnancy: 0–250 mIU/mL
4 to 6 weeks: 100–5,000 mIU/mL
6 to 10 weeks: 4,000–200,000 mIU/mL
10 to 14 weeks: 8,000–100,000 mIU/mL
Second trimester: 4,000–75,000 mIU/mL
Third trimester: 1,000–5,000 mIU/mL
Although a wide range can exist among women, HCG levels do have a typical trajectory during pregnancy:
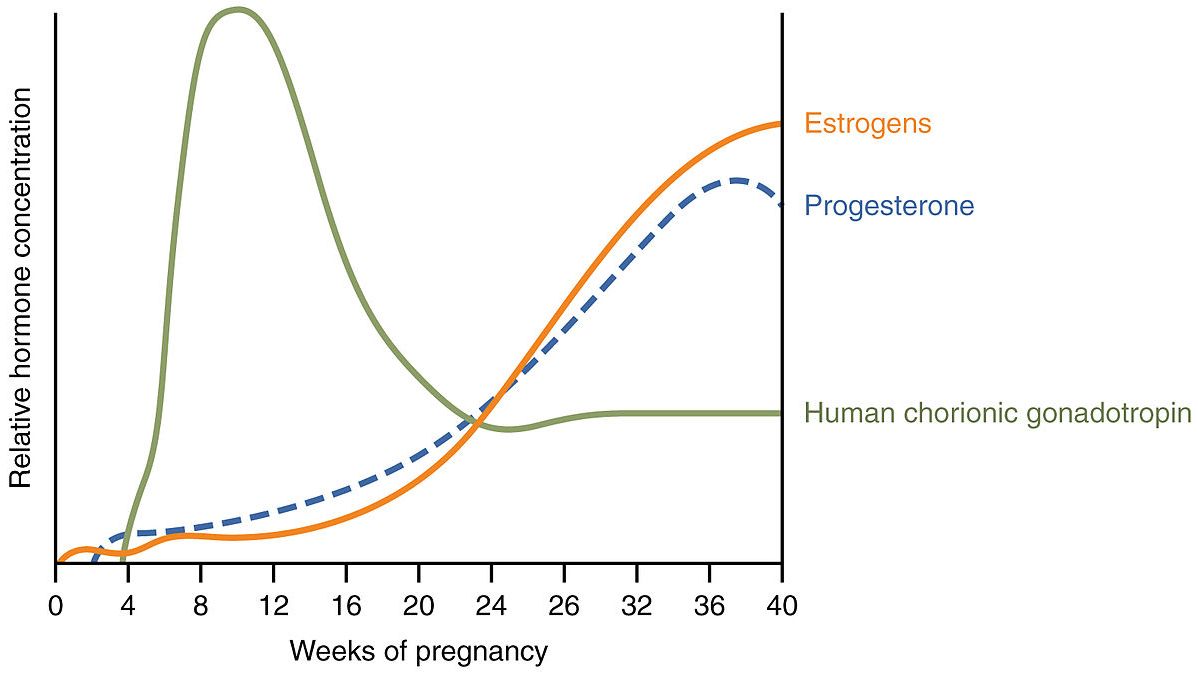
HCG levels increase exponentially during very early pregnancy, after reaching a plateau during the late first trimester. The average peak HCG level is approximately 110,000 mIU/mL and occurs at 10 weeks gestation.
Between 12 and 16 weeks, average HCG decreases rapidly, halving every one to four days until reaching 10% to 25% of first trimester peak values. During the third trimester, HCG levels rise in a gradual but significant manner from approximately 22 weeks until term.
Several studies have shown that rates of rise of HCG are similar in twin pregnancies compared to singleton gestations, with only much higher values seen in triplets or higher.
Doubling in Early Pregnancy
It is very commonly believed that in healthy early pregnancies (up to 8 weeks), HCG doubles approximately every 48 hours. Newer research shows any doubling pattern may be a bit more complicated, as the original data for the 48-hour doubling rule was misleading.
Understanding the exact rise in early pregnancy is important, as health care providers (HCPs) currently use the 48-hour rule to help determine the viability of a fetus in the first trimester, as well as to potentially diagnose a possible asymptomatic ectopic pregnancy.
A slow rate of rise or a drop in HCG levels during the first 8 to 10 weeks of pregnancy usually represents death of trophoblastic tissue and can indicate ectopic or impending miscarriage.
Larger studies of HCG levels were published in the mid-2000's and determined the minimum expected rise of HCG within 48 hours could be as slow as 53% and the pregnancy could still turn out to be viable.
Additional studies indicate doubling time of HCG could take up to three days around 4 weeks of pregnancy and up to five days at 9 to 10 weeks. HCG levels are not as clearly defined after 10 weeks of pregnancy.
Given the large range of normal HCG levels and inconsistent expected doubling times, HCG levels are usually combined with ultrasound evaluation in evaluating the health and viability of an early pregnancy. Further, more than one check of HCG levels is often recommended if an HCP has any concerns.
Discriminatory Level
An HCG “discriminatory level” is often used to aid in determining whether a woman has a potential intrauterine pregnancy when nothing can be seen on transvaginal ultrasound (read First Trimester Viability).
The concept of the HCG discriminatory level was first reported in 1981 when all intrauterine pregnancies included in the study were visible on transabdominal ultrasound at an HCG level greater than 6,500 mIU/mL.
Since the use of transvaginal ultrasound has greatly improved in the last 40 years, the discriminatory level has been set much lower, to 2,000 mIU/mL, since embryonic structures can now be seen earlier. It is currently believed that a gestational sac is always seen by transvaginal ultrasound when the HCG level is greater than 2,000 mIU/ml.
A discriminatory level can also be helpful in the diagnosis of ectopic pregnancy. If a woman has HCG levels much higher than the discriminatory level, but a gestational sac is not seen, then ectopic pregnancy is very likely. This is also important because even if a woman does not yet have symptoms (abdominal pain, bleeding), diagnosing ectopic pregnancy as early as possible can prevent bleeding and rupture complications.
Additional Factors
Certain characteristics, such as smoking, carrying multiples, ethnicity, body-mass index, placental weight, molar pregnancies, hyperemesis gravidarum (debated), and fetal sex may affect HCG levels.
Smoking is strongly correlated with lower HCG levels. Women who immediately stop smoking around 4 to 5 weeks of pregnancy may counteract any negative effects on HCG levels and could eventually develop the same levels as nonsmokers.
Pregnant women carrying girls are reported to have higher HCG levels than those carrying boys; however, exactly how much higher is unclear. However, HCG levels should not be used in early pregnancy to determine the sex of the fetus, as this method is not consistently reliable.

A complete molar pregnancy – an abnormally fertilized egg – tends to have very high levels of HCG, typically greater than 100,000 (a partial molar pregnancy may be within the normal range).
Body mass index may have an affect on HCG early in pregnancy and can cause a slow early rise that may lead HCPs to diagnose a viable pregnancy as potentially nonviable. Researchers have advocated that HCPs take BMI into account when assessing early HCG levels.
For decades, high HCG levels have been linked with nausea and vomiting of pregnancy (NVP). Recent research is stepping away from HCG as a cause of NVP, which is now likely due to numerous factors, with HCG possibly playing only a minor role. It is believed that prior links were mostly coincidental, based on the time NVP begins and HCG levels peak (read Causes and Contributing Factors of NVP).
Action
Not all women are given their HCG levels early in pregnancy. However, for women who are interested, they should talk to their HCP and ask what their level(s) may mean.
Women should understand, however, that trying to make sense of numbers to determine the viability of a pregnancy may cause significant anxiety, and having to wait several days or even a week for answers can be very difficult.
Women should also understand that HCG levels are not an exact science, and are only meant to confirm a possible pregnancy, confirm a miscarriage has completed, and guide HCPs for possible scenarios.
Further, it is likely HCG levels have much better accuracy for determining ectopic and molar pregnancies then determining whether a miscarriage may or may not occur.
Ectopic pregnancy can be a potentially life-threatening condition due to the possibility of hemorrhage. Ectopic pregnancy usually presents with abdominal pain, bleeding, and pain that may radiate to the shoulder. Women should always call their HCP if they experience abdominal pain or bleeding at any point during pregnancy (read Ecoptic Pregnancy).
Women who use cigarettes should ask their HCP for resources to help them quit during pregnancy (read Smoking).
Resources
History of the Pregnancy Test (Harvard University)