Ectopic Pregnancy

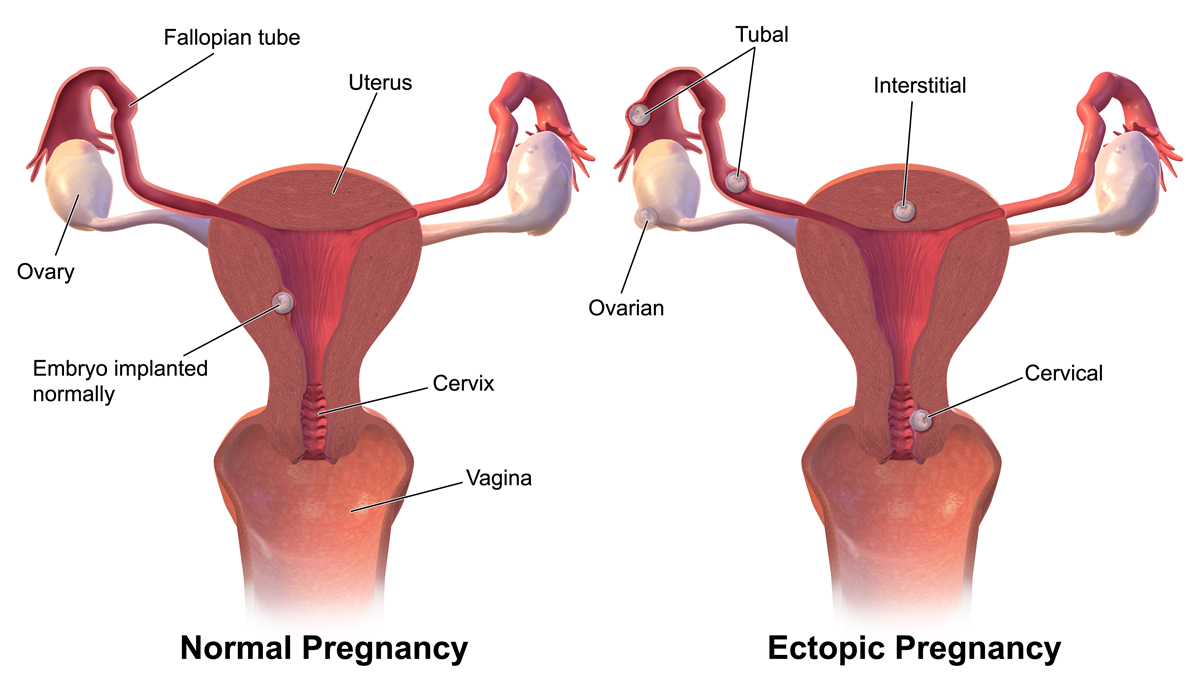
Ectopic pregnancy occurs when a fertilized egg implants in a uterine structure other than the uterine lining (decidua), such as the cervix or Fallopian tube.
Ectopic pregnancy is considered a gynecological emergency because if left undiagnosed and untreated, the developing embryo could cause the Fallopian tube to rupture, which is life-threatening.
Women need to call their HCP anytime in early pregnancy if they are experiencing pain or bleeding; ectopic pregnancy needs to be ruled out.
However, in the event women do not feel any symptoms until their Fallopian tube ruptures, these symptoms can include intense abdominal and pelvic pain, pain that radiates to both shoulders, nausea, vomiting, faintness, and shock. If women experience any of these symptoms during pregnancy, they need to seek emergency care immediately.
If ectopic pregnancy is diagnosed prior to rupture, medication and surgical options are available, all of which are safe and effective; most women go on to have future successful pregnancies.
Background
Ectopic (“out of place”) pregnancy occurs when a fertilized egg implants and grows outside the main cavity of the uterus, usually in a Fallopian tube. A fertilized egg can also implant in the cervix, ovary, abdominal cavity, prior cesarean scar, or where the uterus and Fallopian tube meet, but these are very rare.
Ectopic pregnancy is a form of pregnancy loss, because ultimately, the embryo cannot survive as the necessary blood supply is not available. Additionally, even though the embryo may survive for a few weeks, the Fallopian tube can rupture as the embryo grows, a life-threatening complication for the woman.
About 1 in 50 pregnancies (2%) in the United States and 11 in 1,000 pregnancies (1%) in the United Kingdom are ectopic, which averages to about 75,000 and 10,000 pregnancies each year, respectively.
Signs, Symptoms, and Complications
Ectopic pregnancy is considered a gynecological emergency as it can be life-threatening, and accounts for up to 6% of all pregnancy-associated deaths.
Women with an ectopic pregnancy commonly present with abdominal/pelvic pain and vaginal bleeding between 6 and 10 weeks. Although these are considered common symptoms in normal early pregnancy, women are advised to call their HCP anyway, as ectopic pregnancy needs to be ruled out.
It is important that women recognize the signs of tubal rupture as some women may have no symptoms until rupture occurs (especially in young, otherwise healthy women). Rupture usually occurs between 6 and 16 weeks and always requires immediate surgery.
Even more critically – women (or the woman’s partner) need to immediately inform the physician at the emergency department that the woman is, or may be pregnant, or that ectopic pregnancy is possible. This avoids any delay in diagnosis and can result in the prevention of severe internal bleeding.
The incidence of ectopic pregnancies that rupture is around 18%, and presumably rises with increasing gestational age.
Causes/Risk Factors
There is no way to prevent an ectopic pregnancy, but certain risk factors have been documented that appear to increase the chances a woman may experience an ectopic pregnancy.
Although the exact cause or mechanism for why ectopic pregnancy occurs is not known, it is thought to potentially be a result of "delayed transfer", or slower travel through the Fallopian tube, likely due to inflammation.
This is further corroborated through an analysis of risk factors, which all appear to increase inflammation of the uterus and other pelvic organs (and as such, inflammation is the leading theoretical cause of ectopic pregnancy):
Previous ectopic pregnancy
Inflammation or infection (STI)
Fertility treatments (*the very first IVF pregnancy was ectopic)
Previous tubal, pelvic, or abdominal surgery (including cesarean section)
Use of certain types of birth control (IUD)
Smoking (as much as 1/3 of all ectopic pregnancies are associated with smoking)
Endometriosis
Age may be an additional risk factor, as the incidence of ectopic pregnancy is slightly higher between 35 and 44 years (2.7 per 100), than for all women combined (2 per 100).
However, avoidance of these risk factors does not guarantee a woman will not experience an ectopic pregnancy. Further, about one half of all women who have an ectopic pregnancy do not have any known risk factors.
Diagnosis
When a woman presents with symptoms indicating possible ectopic pregnancy, standard tests include a pelvic exam, ultrasound, and blood tests.
Ectopic pregnancy is usually a diagnosis of exclusion – meaning, the HCP rules out other causes of the pain and bleeding first, as ectopic pregnancy can be difficult to see on ultrasound, especially earlier than 5 weeks. Tests (HCG levels, ultrasound) may need to be repeated every few days to confirm the diagnosis.

An ectopic pregnancy has a poorly developed placenta with less blood supply; therefore, HCG does not rise as quickly compared to an intrauterine pregnancy. However, HCG is not always a good indicator of potential ectopic pregnancy as studies are conflicted whether there is a true pattern regarding rise or fall.
The best evidence via ultrasound is no gestational sac 38 days or more after the last menstrual period (5 to 6 weeks of pregnancy). At this point, a gestational sac should always be seen, and therefore ectopic pregnancy is considered very likely.
In some cases, laparoscopic surgery may be necessary to confirm diagnosis, which can also be used to treat the ectopic pregnancy at the same time (see below).
Management Overview
Unfortunately, an ectopic pregnancy always ends in pregnancy loss. Without treatment, it can lead to heavy bleeding and even death for the woman, especially if the tube ruptures.
Researchers indicate the primary goal should be to successfully treat ectopic pregnancy as soon as possible to avoid serious complications, while also minimizing major interventions (e.g. unnecessary surgery).
Depending on many factors, ectopic pregnancies can require no treatment (*rarely), be treated with medication (methotrexate), or require surgery. All options should be openly discussed with an HCP. At least one study indicated that HCG level may be a good indicator of the most likely successful option (the lower the number, the higher likelihood surgery may be avoided).
It is estimated that between 15% to 40% of ectopic pregnancies can be treated with medication and without surgery (if diagnosed early).
Although there are documented cases of some ectopic pregnancies resolving on their own, watching and waiting (expectant management) is considered very risky, especially with the excellent safety and success rates of medical or surgical treatment.
However, ectopic pregnancy management during the COVID-19 pandemic has revealed higher success rates than expected following expectant management, without increasing the rates of complications. It is possible that in women with low or declining HCG levels, expectant management may be a viable option. (Note: Women who believe they may have an ectopic pregnancy should always call their HCP instead of waiting for the pregnancy to resolve on its own.)
Rarely, the embryo is expelled by the Fallopian tube before rupture occurs. This is called a "tubal abortion." Women who have tubal abortion can develop either severe bleeding requiring surgery, or minimal bleeding that may not require treatment.
Women diagnosed with an ectopic pregnancy should talk to their HCP about the risks and benefits of all their management options.

Management – Medication
An injection of methotrexate is the most common medical method used to resolve an ectopic pregnancy that has not ruptured, is located in the Fallopian tube, and is still small in size.
The drug stops rapidly dividing cells from growing (the drug is also used in cancer treatment) – usually in one dose – which ends the pregnancy. The pregnancy is then absorbed by the body over a period of four to six weeks. This method, if successful, can also save the Fallopian tube.
In general, side effects are not common, but most women experience abdominal cramping and bloating for a few days. Additional possible side effects include nausea, vomiting, diarrhea, and mouth sores. These effects can usually be avoided or controlled by monitoring the dosage. Methotrexate is not recommended if women are currently breastfeeding.
It is possible for the methotrexate to be injected into the ectopic sac to avoid full systemic absorption of the drug, but this does not appear to have any major advantages, and the injection may risk rupturing the tube.
Levels of HCG in the blood are taken before and after treatment. If HCG levels do not fall as expected, some women may require a second dose. HCG levels are monitored continuously to make sure levels falls to zero and the ectopic pregnancy has resolved.
Methotrexate has a high success rate; however, if HCG levels do not fall after a second dose, or if rupture is suspected, surgery is then required.
After methotrexate use, women are advised to avoid sex, prolonged exposure to sunlight, heavy exercise, and alcohol. Prescription pain medication such as ibuprofen and other nonsteroidal anti-inflammatory drugs need to be avoided as they can interfere with methotrexate. Women are usually advised to take acetaminophen (Tylenol®) for any discomfort after treatment.
Management – Surgery
Surgery may be needed to manage an ectopic pregnancy, even if the tube has not ruptured. It is also possible that surgery can remove the tissue without removing the Fallopian tube. However, it is common for the entire tube to be removed.
Surgery is either completed through the abdomen or laparoscopically, but both require general anesthesia. In laparoscopic surgery, the HCP will remove the embryo with surgical instruments, including a camera, through very small openings in the abdomen. In the abdominal version of the surgery, an incision is made through the abdomen so the HCP can directly see and remove the tissue and/or tube.
Although surgery is very effective at removing all tissue, it is possible that if HCG levels do not lower enough (or all the way) after surgery, then a dose of methotrexate may also be given.
Recovery from surgery is different for all women, but most can return to normal activities within a week of surgery. Women who had laparoscopic surgery may recover sooner than those who had an abdominal incision.
Risks/side effects of surgery can include pain, fatigue, bleeding, and infection. It is advised that women call their HCP if they experience severe pain, bleeding, or a fever.

Action
Women who experience abdominal or pelvic pain and/or bleeding during early pregnancy should call their HCP for immediate evaluation. Although these are common symptoms of early intrauterine pregnancy, ectopic pregnancy should always be ruled out.
For women diagnosed with an ectopic pregnancy, they should have a risks and benefits discussion with their HCP regarding all their management options so they can fully participate in the selection of the most appropriate treatment for their own health.
Additionally, for some women, ectopic pregnancy can be traumatic, regardless of management method. HCPs can recommend counseling and/or support groups that can help women as they mentally and emotionally go through the management process, as well as recovery.
Women who have experienced an ectopic pregnancy should consider sharing their experience below. This can be incredibly value for other women in early pregnancy so they may better understand the warning signs as well as the process they may go through from diagnosis to recovery.
Resources
Ectopic Pregnancy Booklet (The American Society of Reproductive Medicine)
Ectopic Pregnancy (American College of Obstetricians and Gynecologists)
Ectopic Pregnancy (Miscarriage Association)
The Ectopic Pregnancy Trust (United Kingdom)