Preeclampsia

Preeclampsia is a vascular condition during pregnancy that manifests primarily as high blood pressure, but can also include protein in the urine, sudden swelling in the face and hands, headache, vision changes, sudden weight gain, and abdominal pain. When preeclampsia is diagnosed early, its management can prevent serious complications during pregnancy and in the postpartum period.
However, the condition is associated with severe complications when untreated or recognized late, such as in the postpartum period.
The only way to prevent and most effectively manage the condition is through screening. Screening includes a detailed medical history and the monitoring of blood pressure, weight, urine tests, and symptoms such as headache, swelling, and vision changes.
It is important that women understand and recognize these symptoms for themselves, as mild to severe preeclampsia can progress to full eclampsia very quickly ― even in a matter of days, and prenatal appointments can vary between 2 to 4 weeks in the second half of pregnancy (and 6 weeks postpartum).
Women should call their HCP immediately if they recognize any of the signs or symptoms described in detail below.
Background
Preeclampsia is a pregnancy-specific, serious vascular (blood vessel) disorder that can affect both the woman and baby, and virtually every organ system in the mother.
Preeclampsia is a heavily researched condition during pregnancy, but its definition, diagnosis criteria, screening recommendations, and management guidelines remain variable. While there is no effective treatment during pregnancy (other than delivery), researchers are beginning to focus on its prevention through screening and assessment of risk factors.

The incidence of preeclampsia in the United States has recently increased by 30% (total of 4% to 8% of all pregnancies), which has been attributed in part to an increase in pregnant women that have known risk factors for the condition (see Risk Factors, below).
Causes
Preeclampsia was once called “the disease of theories”. It is a major concern in obstetrics due to its potential complications and because the cause is still unknown, although it appears the blood vessels and placenta may be the primary factors.
The current leading theory, supported by both human and animal studies, is that preeclampsia begins as a vascular disorder within trophoblastic cells (which create the placenta) that leads to inflammation and oxidative stress. This is thought to occur in the following manner:
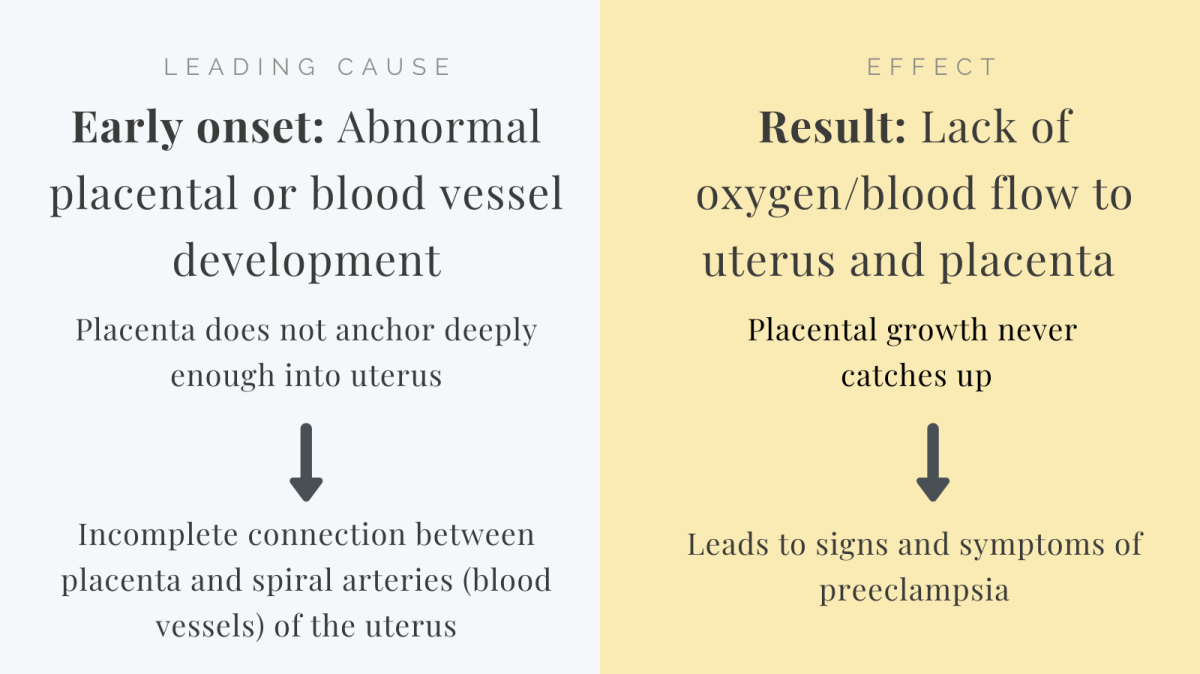
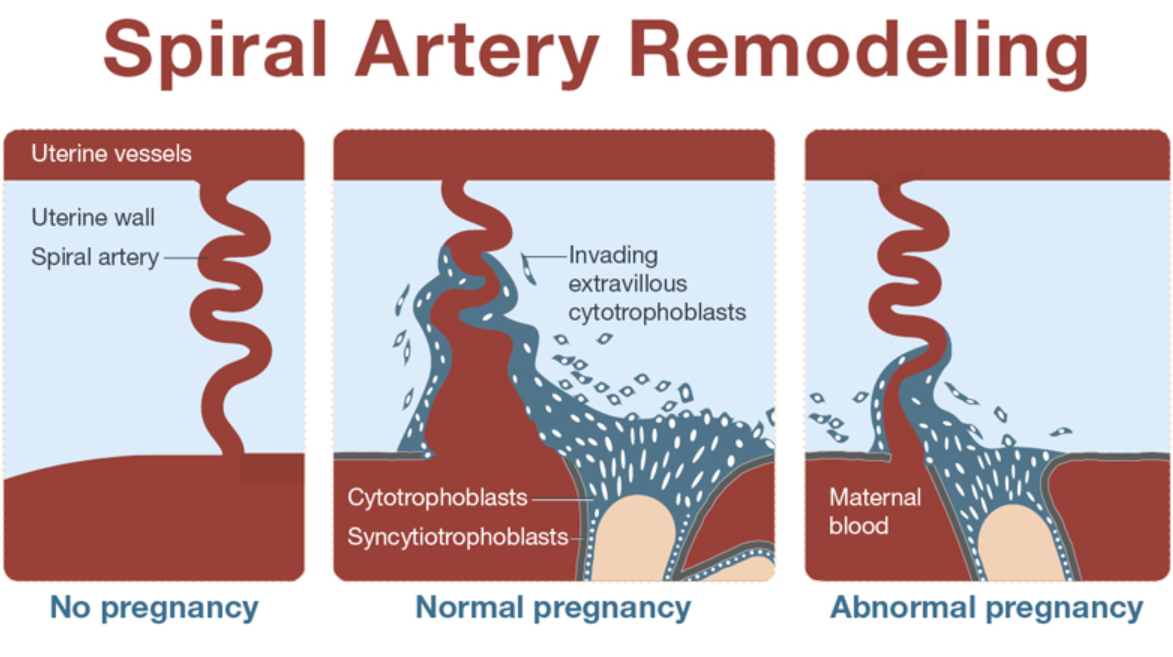
Trophoblasts are responsible for oxygen exchange between the mother and fetus through the placenta. Very early in pregnancy, these cells help to remodel the uterine spiral arteries so these arteries can supply nutrients to the placenta and fetus. This results in a necessary and dramatic increase in blood supply to both organs.
A failure of the remodeling of these arteries in the uterus results in a restriction of blood supply to the placenta because the connection between mother and placenta is inadequate – the arteries fail to anchor deeply enough.
The placenta then releases “antiangiogenic factors” (agents that inhibit blood vessel growth) into the mother’s circulation as its own cells die from a lack of oxygen and nutrients. These factors harm the mother’s own blood vessels because her system cannot clear them.
Blood vessel harm by these angiogenic factors causes them to constrict and leak, leading to the hallmark signs of high blood pressure and swelling. These factors also harm other organs, leading to the various other signs and symptoms of preeclampsia (i.e. damaged kidneys release protein).
The recognition of this process in the research and medical community has shifted the diagnosis focus away from protein in the urine and to the recognition of these harmful factors in the woman’s blood to diagnosis the condition.
One study from November 2020 found that women with severe angiogenic imbalance had higher rates of adverse pregnancy outcomes and progression to preeclampsia when compared with patients with no or mild angiogenic imbalance.
The actual cause of the failure of the above described remodeling process is not known, but numerous theories are being investigated: environmental exposures, nutrition, autoimmune disorders, inability to adapt to vascular changes, hormonal imbalances, pre-existing diabetes, prostaglandins, oxidative stress, chronic blood pressure, as well as the body’s inability to adjust to the early fluid changes of pregnancy. Preeclampsia risk is likely a combination of these factors.
At least two recent studies have found that the gene sFLT1 may be an identified marker for preeclampsia risk. This protein interferes with the activity of vascular endothelial growth factor (VEGF), which is an important regulator of blood vessel development.
Interestingly, the same study identified that pregnant women who were vitamin D deficient had significantly higher expressions of sFLT1 and lower expression of VEGF in the placenta than women who were not vitamin D deficient.
In late onset preeclampsia (noticed near term), the placenta appears to be growing normally but is compressed; the mother then experiences high blood pressure and other signs/symptoms.
High Blood Pressure
The first hallmark sign of the potential development of preeclampsia based on the roadmap above is high blood pressure. Blood pressure is the pressure of the blood against the blood vessel walls each time the heart contracts (squeezes) to pump the blood throughout the body. HCPs will take a woman’s blood pressure during every prenatal visit to attempt to identify even the earliest changes.
Preeclampsia is defined as the new onset of high blood pressure (more than or equal to 140/90 mmHg) on two occasions, at least four hours apart, or blood pressure readings of more than or equal to 160/110 mmHg in a woman with previously normal blood pressure.
Preeclampsia can be especially difficult to detect in women who have a history of high blood pressure (hypertension) before pregnancy, yet it is also more likely to occur in these women, which is known as superimposed preeclampsia.
In November 2017, the American College of Cardiology and the American Heart Association updated the definition of chronic hypertension (before pregnancy) to be more than or equal to 130/80 mmHg instead of more than or equal to 140/90 mmHg. This allows for early monitoring of a higher number of women who may develop preeclampsia.
Women can also have normal blood pressure prior to pregnancy but develop high blood pressure during pregnancy that does not yet fulfill criteria for preeclampsia. Gestational hypertension, a “flag” and potential precursor to preeclampsia, occurs when a woman who previously had normal blood pressure develops high blood pressure when she is more than 20 weeks pregnant but has no protein in her urine. Approximately 25% of women with gestational hypertension go on to develop preeclampsia.
In the general population, hypertension is sometimes referred to as a "silent killer" because most people cannot “feel” their blood pressure going up. Although HCPs monitor blood pressure at every appointment, some women may need to take and record their own blood pressure at home.
In many cases, gestational hypertension does not harm the mother or fetus, but complications have increased in recent years, such as preterm birth. In general, hypertensive conditions are associated with not only preeclampsia, but eclampsia, placental abruption, stroke, and/or a need for immediate delivery. Hypertension can also affect the blood vessels in the umbilical cord, leading to a possible decrease in oxygen and nutrients to the fetus.
Severe hypertension (160 mm/110 mm HG or higher) that lasts more than 15 minutes in both pregnant and postpartum women with preeclampsia or eclampsia is a hypertensive emergency, is considered life threatening, and needs to be treated immediately.
Proteinuria
Traditionally, proteinuria was considered a mandatory sign of preeclampsia, but the presence of protein in a woman’s urine is no longer needed to make the diagnosis, especially when early attempts are made to diagnosis the condition.
Further, pregnant women who are older, obese, undergoing in vitro fertilization, or carrying more than one fetus may have protein excretion that is higher than current established thresholds but do not have preeclampsia.
Proteinuria occurs when proteins that are normally present in the blood through the healthy, normal filtering process of the kidney, spill into urine. The process that causes preeclampsia damages the filtering ability of the kidney, resulting in proteinuria.
The screening tool used to assess the level of protein in the urine is known as a dipstick test and is done in an HCP’s office by dipping a test strip into a cup of urine. This test remains routine; proteinuria in general indicates inflammation in the body, and could also result in preterm labor or premature rupture of membranes, as well as preeclampsia.
Some HCPs may request a urine collection for 12 or 24 hours to determine the exact quantity of protein in the urine.
Additional Signs and Symptoms
Since there is no one blood test yet than can definitively determine whether a woman has preeclampsia, the diagnosis relies heavily on the awareness and identification of its related symptoms, such as high blood pressure and proteinuria, as described above.
There are also additional signs and symptoms women need to recognize, especially since prenatal appointments are generally two to four weeks apart.
Mild preeclampsia can progress quickly, sometimes in a matter of days. Women should learn to recognize the signs and symptoms of preeclampsia for earlier diagnosis - including after delivery.
A woman may have preeclampsia when she presents with signs and symptoms that indicate an inflammatory process is occurring: high blood pressure, swelling (face/hands/legs), rapid weight gain (from fluid), headache, and/or vision changes (severe headache and vision changes indicate an emergency, see below).
These signs and symptoms occur because a pregnant woman's cerebral vasculature is highly vulnerable to the adverse effects of preeclampsia.
Blood pressure of 140/90 mmHg or higher along with any of the following symptoms can indicate preeclampsia and women need to describe these to their HCP.
Excessive swelling (edema) of the face or hands: Although swelling of the hands, feet, and legs is common during pregnancy, preeclampsia results in sudden swelling, to include the face and around the eyes. Damage to the mother’s blood vessels results in significant fluid leaking into various compartments of the skin. Normal pregnancy-related swelling is usually gradual, and does not usually occur in the face (read more).
Weight gain: A sudden weight gain of more than 3 to 5 pounds in a week, or 2 pounds in a matter of days is a flag as this indicates fluid retention, a result from the same process described above for sudden swelling.
Headaches: Preeclampsia can include dull or severe throbbing headaches, that may include vision changes and nausea and/or vomiting. Women who experience a severe headache need to call their HCP for a same-day visit. Among pregnant women with no history of a headache and the onset of new or atypical headache that does not respond to over-the-counter medications, it is estimated one-third have preeclampsia.
Vision changes: Vision changes are one of the most serious symptoms of preeclampsia. Women may observe flashing lights or spots, increased sensitivity to light (photophobia), blurry vision, or temporary blindness. It is theorized these changes are caused by central nervous system irritation or fluid buildup in the brain or eye that puts pressure on the retina.
First documented in 1855, visual symptoms affect 25% to 100% of patients with severe preeclampsia and 50% of patients with eclampsia; blurred vision is the most common vision-related symptom.
Most of the visual disturbances during pregnancy that are the result of hypertension and preeclampsia tend to reverse in the postpartum period, but still require immediate medical attention.

Shortness of breath: Shortness of breath is a normal symptom of pregnancy, especially in the first trimester due to the various early changes of the circulatory system. When it is associated with preeclampsia, it is due to sudden swelling and damage to the blood vessels that results in less oxygen flow throughout the body. It can also be a sign of pulmonary edema due to dramatic fluid buildup.
Decrease in urination: A decrease in urination is the result of dehydration, again, as a result of fluid buildup.
Nausea or vomiting: Nausea and vomiting can accompany headache and vision changes, or present suddenly after mid-pregnancy.
Upper abdominal pain: Preeclampsia, or a related condition known as HELLP syndrome, can cause shoulder pain (“referred pain”) which radiates on the right side and from the liver.
HELLP syndrome occurs when the liver and blood-clotting systems are not functioning properly. Approximately 30% to 50% of women with eclampsia also have HELLP syndrome. HELLP stands for (Hemolysis, Elevated Liver enzymes, and Low platelet count).
These same signs and symptoms of preeclampsia can also occur in the postpartum period.
Complications (& Eclampsia)
Expecting mothers rarely die from preeclampsia, especially when diagnosed and treated early. However, it is considered life-threatening due to the wide and extensive systemic damage it produces within the body. High blood pressure alone can increase the risk of heart and kidney disease, stroke, placental abruption, postpartum hemorrhage, and seizures.
About 1 in 200 women with untreated preeclampsia develop eclampsia, which usually results in seizures. Seizure can also occur with preeclampsia and in the postpartum period.
Management of an eclamptic seizure includes supportive care to prevent recurring seizures, as well as serious maternal injury that may result. Magnesium sulfate may be administered and immediate delivery is often recommended.
It is currently estimated that an eclamptic seizure will occur in 2% of women with severe features who are not receiving magnesium sulfate and in less than 0.6% of those receiving magnesium sulfate.
The exact reasons why a seizure may occur in either preeclampsia or eclampsia is not well understood. The leading theory indicates the blood-brain barrier may be disrupted due to the circulating angiogenic factors described above.
In a small percentage of women with preeclampsia, liver damage may also occur. This damage could be the result of two possible conditions: HELLP syndrome (described above) or Acute Fatty Liver of Pregnancy (AFLP). Some women may experience both.
There is debate whether AFLP is related to preeclampsia or should be considered a separate entity, but it is estimated that 50% of women with AFLP have hypertension and proteinuria, similar to preeclampsia.
The cause of AFLP is not known with complete certainty, but it is believed that defective metabolism of fatty acids occurs, which leads to a build up of these acids in the liver. AFLP can cause nausea, vomiting, abdominal pain, and/or jaundice.
AFLP is rare, occurring in approximately 1 in 10,000 pregnancies, but can be fatal if not treated (supportive management for symptoms until delivery becomes necessary).

Risk Factors
Risk factors for preeclampsia include:
Carrying more than one baby
Use of artificial reproductive technology
High blood pressure prior to pregnancy
Family history of hypertension or cardiovascular disease
Cardiac problems
Diabetes
Kidney disease
Getting pregnant older than 40 years of age
Antiphospholipid antibody syndrome and other autoimmune disorders
There is also some evidence that the woman’s immune reaction to the father’s sperm may also play a role
It is assessed that failure of trophoblast cells to remodel the spiral arteries may be genetic. However, many cases of preeclampsia occur in women with no known history of the condition, and therefore other risk factors likely also play a role.
Preeclampsia may recur in a subsequent pregnancy in an estimated 20% of women who had preeclampsia in a prior pregnancy. However, this is highly variable depending on the gestational age of the first pregnancy, number of prior pregnancies, a woman's age, and the above risk factors.
Management
The main goal in the management of high blood pressure and preeclampsia is to control the condition and its symptoms long enough for a safe and healthy delivery.
HCPs will continue to monitor and conduct:
Blood tests to assess the woman’s liver and kidneys, clotting ability, and red blood cells
Checks of weight and blood pressure
Ultrasound/Fetal heart rate assessments
Physical examinations for swelling in the mother's face, hands, or legs, as well as abdominal pain
Urine dipsticks to assess proteinuria and infection
Women with severe hypertension may be advised to take medication or monitor their blood pressure at home.
Magnesium sulfate is often recommended for the prevention of eclampsia/seizures in women with severe preeclampsia.
Corticosteroids may be given to help the baby’s lungs mature in the event delivery is anticipated.
Immediate delivery is recommended if the condition worsens to the point where the health of mother and/or baby is severely threatened. The condition usually dramatically improves with the delivery of the placenta – but not always, and women are advised to continue monitoring for symptoms in the postpartum period.
Although each individual case is different, vaginal delivery (through induction) and the use of an epidural remain viable options for women with preeclampsia.
Postpartum
Most women begin to improve within one to two days after delivery, and blood pressure returns to normal within a few weeks.
On rare occasions, preeclampsia can occur after delivery, known as postpartum preeclampsia, which can be diagnosed within 48 hours after delivery but could also present up to six weeks later.
Women who were diagnosed with either preeclampsia or eclampsia during pregnancy have a higher risk of developing either in the postpartum period. Postpartum preeclampsia carries the same risks as during pregnancy and is still considered life-threatening, requiring immediate treatment.
In addition, according to at least one study published in August 2021, women who were diagnosed with preeclampsia have a higher chance of being diagnosed with chronic kidney disease (19% vs expected 3% in women in childbearing age). The authors noted this indicates women who experienced preeclampsia should receive follow up care by a health care provider in the postpartum to assess possible kidney damage or risk of future complications.

Women need to be aware of the signs and symptoms described above and need to seek emergent care at a hospital if they experience one or more signs/symptoms, especially if they were previously diagnosed with preeclampsia, eclampsia, or high blood pressure.
Women should call their HCP even if they are hesitant about their symptoms, and should also not be afraid to seek help if they feel they need it.
Prevention
The best away to manage preeclampsia is to prevent it or diagnosis it as early as possible. Although researchers are still attempting to determine a cause, there are screenings available that can help those most at risk.
According to the American College of Obstetricians and Gynecologists, taking a detailed medical history is the best and only recommended screening for preeclampsia risk in the first trimester.
In some countries, a blood test (not yet available in the United States) measures the ratio between two proteins found in the placenta (sFLT and PIGF) to predict which women suspected of preeclampsia will develop the condition in the near future.
Women with blood pressure concerns can monitor their blood pressure from home and keep a log they can share with their HCP. For accuracy, blood pressure readings should be taken in the sitting position, with the cuff positioned on the left arm at the level of the heart.
Daily low-dose aspirin (LDA) is of significant research interest due to its potential to lower preeclampsia risk in high-risk women (although results remain inconsistent).
A study published in September 2021 found that daily low-dose aspirin during pregnancy was associated with lower risks of serious perinatal outcomes for individuals at increased risk for preeclampsia, without evident harms. Trial data derived from more than 25,000 pregnant individuals randomized to daily aspirin use did not reveal any serious harms.
A study published in July 2021 found that aspirin significantly slowed down metabolic gestational age by 1.27 weeks and therefore slowed down the advancement of preeclampsia.
Despite some relative inconsistency, international guidelines, including those from the World Health Organization, have reported that a dose of 75 to 100 mg of aspirin should be prescribed from 12 weeks of pregnancy until delivery in women considered at high risk of preeclampsia.
Other guidelines indicate LDA should be prescribed prior to 12 weeks of pregnancy based on the timing of trophoblast invasion. To date, the optimal timing and/or dose of LDA has not been determined.
Women should never take any medication for the prevention or management of preeclampsia without speaking to their HCP.

According to an April 2021 meta-analysis of 15 studies and more than 2,000 participants, low-molecular-weight heparin (LMWH) decreased the incidence of preeclampsia and other placental-related complications in high-risk women and when treatment was started before 16 weeks’ gestation.
Combined treatment with LDA was associated with a significant reduction of PE compared with LDA alone. However, further research is necessary to the low-quality evidence overall. Of note, no increased risk of hemorrhage or placental abruption was found with LMWH alone or in combination with LDA.
Action
Women need to be aware of the emergent signs and symptoms described above and need to seek emergency care at a hospital if they experience one or more signs/symptoms, especially if they were previously diagnosed with preeclampsia, eclampsia, or high blood pressure.
Women should never hesitate to call their HCP if they have any questions or concerns.
Women should make sure their HCP is aware of their headache history, as this helps HCPs identify patients who may be at an increased risk of preeclampsia and related hypertensive disorders of pregnancy.
Women should also consider sharing and submitting their experience below regarding high blood pressure, preeclampsia, or eclampsia. This can help other women learn additional perspectives regarding this concern, help them be more prepared, give them additional information to look out for, and help them have a more in depth discussion with their HCP.
These conditions can be scary for some women, so if women have the ability to hear other women's experiences (including positive), they can feel less stress and anxiety.
Partners/Support
Partners/support of pregnant women can help women monitor their blood pressure at home if this was recommended. Although women may not need assistance if they are using a machine, partners can help remind women to check their blood pressure often.
Partners/support should also recognize the outward signs of preeclampsia, especially in a postpartum woman (read above). It is possible that partners or other support/family members may notice sudden swelling in the face, hands, or legs faster than the pregnant woman.
Resources
The California Preeclampsia Toolkit (2014)
Preeclampsia and High Blood Pressure During Pregnancy (American College of Obstetricians and Gynecologists)
The Preeclampsia Foundation is a non-profit organization that provides patient education and support for people whose lives have been or will be affected by preeclampsia: mothers, babies, fathers, and their families.
Action on Pre-Eclampsia aims to raise public and professional awareness of pre-eclampsia, improve care, and ease or prevent physical and emotional suffering caused by the disease (United Kingdom).