Musculoskeletal System

Connective tissues of the body loosen and stretch to accommodate the growing uterus and to allow the baby to pass through the bones of the pelvis during vaginal delivery.
This loosening, while necessary, causes loosening and stretching of most other connective tissues – including the ribs – and can cause other issues such as back, pelvic, joint, and ligament pain, along with a risk of potential injury.
Background
Various types of connective tissue support the body's ability to move; this tissue can undergo extensive change or “remodeling” during pregnancy to adjust to alterations in weight, posture, center of gravity, and stability.
The musculoskeletal system comprises of the bones, muscles, cartilage, tendons, ligaments, and joints that provide shape, form, and movement of the body.
Ligament: Strong connective tissue that hold two bones or organs together in place like straps or ropes (such as the round ligament of the uterus)
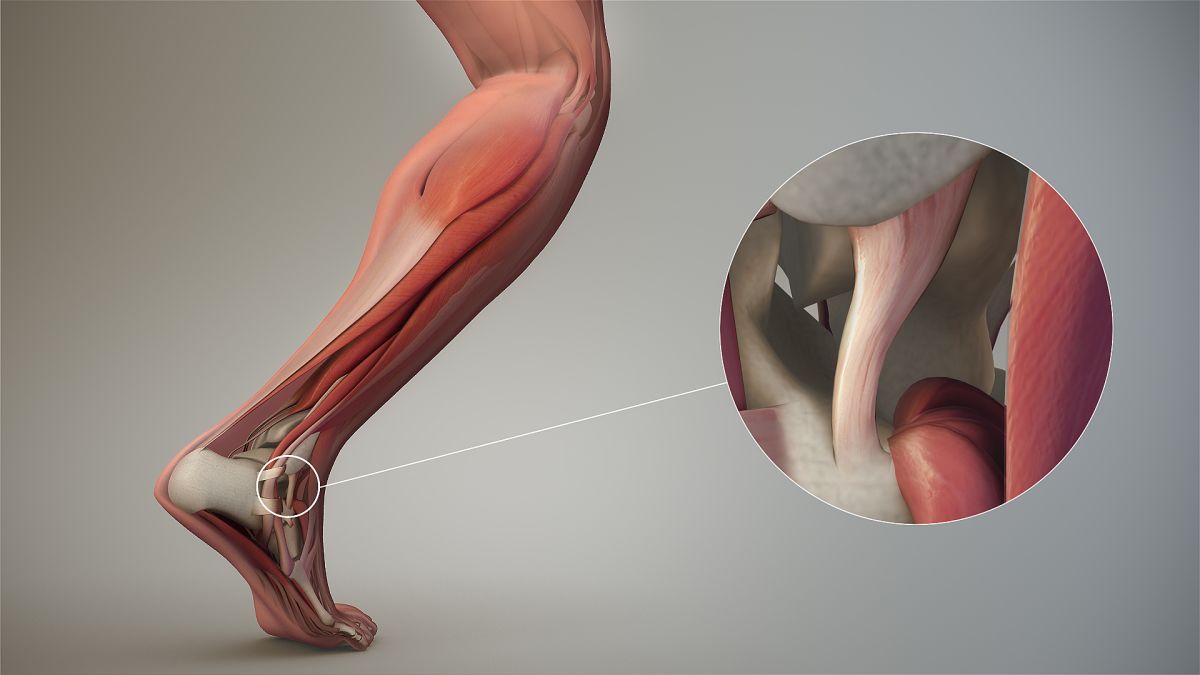
Tendon: Highly organized connective tissue that connects muscle to bone; bends at the joints
Cartilage: Fibrous tissue that provides support on bony areas of the body where there is a need for flexibility
Joint: Defined as a point where two bones articulate or make contact
Bones, muscles, and joints work together in a coordinated way to stabilize the body during movement. When they become loose during pregnancy, instability becomes a new core component of pregnancy and can cause potential injury through exercise, falling, and tripping, or even moving or changing positions too quickly.
Loosening
Relaxin plays an integral role in the remodeling and healing of multiple tissues of the musculoskeletal system, to include the cervix.
Relaxin is produced by the corpus luteum around six weeks of pregnancy to help loosen and expand the pelvic bones, muscles, joints, and ligaments. The placenta produces relaxin after the corpus luteum degenerates.
Although not every type of connective tissue remodels during pregnancy, at least one study illustrated that even the index finger demonstrates a large increase in joint laxity by the third trimester.
Relaxin is also responsible for the loosening of the ligaments in between the ribs. The rib cage spreads out during pregnancy due to the enlarging uterus pushing up the diaphragm. This can cause women to require a larger bra band size (not just cup size).
However, not all research has found a loosening effect across all connective tissue (such as tendons), therefore degree of remodeling may be dependent upon type of tissue. It is also possible that some tendons lengthen, as opposed to loosen, which could also cause potential injury.
Muscles and Joints
The tissues, ligaments, and joints of the female reproductive tract and pelvis change significantly to allow for fetal growth and labor and delivery, but this change can also cause joint pain.
Joint pain can begin early in pregnancy as relaxin levels peak in the first trimester then stabilize to term; relaxin's effects appear to be mostly concentrated around the pelvic region.
However, although relaxin is often cited as a reason for joint and lower back pain, the association between circulating levels of relaxin and joint pain during pregnancy is debated, and many studies have not confirmed this relationship despite its 10-fold increase in the first trimester. The timing of when certain symptoms appear and increased relaxin levels in the blood do not always correlate.
Regardless, joint looseness itself can cause discomfort, hand and wrist pain, pelvic and joint pain, pain of the entire back, and misalignment of the spine. Other factors such as weight gain, posture change, increased weight to the abdomen, fatigue, and growth of the uterus may also play a role, rather than just relaxin.
Further, as pregnancy progresses, the round ligaments of the uterus also become softer, stretch, and cause round ligament pain.

Additionally, both the lumbar and hip extensors must work harder than prior to pregnancy, even just to stand. The hip joints can experience a load almost three times the normal value, and the knee and pelvic joints can experience a more than doubling of normal value.
By the last trimester, the hip abductors, hip extensors, and ankle joints must use more energy to support not only walking, but the different way in which women may change how they walk during pregnancy (slower, with weight toward the heels).
Some women complain of clicking or popping of the lower back and hip joints in and out as they walk or change position.
The changes above may also lead to a permanent change in foot size, and the potential development of carpel tunnel syndrome in the wrists (read Hands and Feet).
Joints should return to normal within one to three months postpartum, but up to a third of women may still have symptoms beyond this time frame.
Pelvic Joints
There are four pelvic joints: the pubic symphysis, two sacroiliac joints, and the sacrococcygeal joint. These joints are relaxed during pregnancy, allowing them to loosen, stretch, and increase in width.
The pubic symphysis and sacroiliac joints are particularly affected during pregnancy and can lead to pelvic and low back pain. The widening of the symphysis pubis is visible on imaging as early as the first trimester and becomes maximum near term.
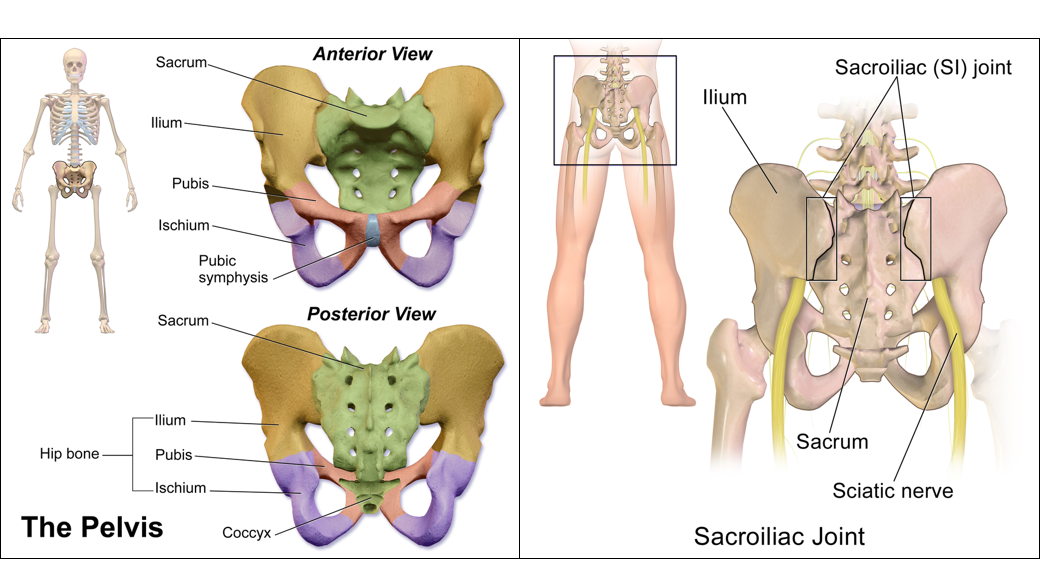
Pelvic girdle pain (PGP) specifically indicates pregnancy related pain in the lumbosacral, sacroiliac, and pubic symphysis joints.
PGP and back pain during pregnancy are often discussed together, but have important differences. They are considered two, distinct entities with different treatments, but some women may experience both at the same time.
About 25% of all women postpartum suffer from PGP during pregnancy, labor, or postpartum, and 5% to 8% have such severe symptoms it leads to disability.
Several risk factors for PGP have been identified, such as possible genetic predisposition, more than one pregnancy, a previous history of pelvic trauma, higher BMI, elevated relaxin levels, abnormal pelvic girdle size, and difficult labor and delivery.
During acute episodes of PGP, brief rest and lying in bed can be helpful, as well as avoidance of exercise or certain everyday activities that will worsen symptoms.
Pregnant women who experience joint pain in the back and pelvic area should be evaluated by their HCP. It is also very important that HCPs rule out possible injury or other causes that may manifest as back/pelvic pain (i.e. urinary tract infection).
Bones
Researchers are still learning more about what happens to a pregnant woman’s bones during pregnancy. It is theorized that because the calcium transfer from the woman to the fetus is so fast and so intense in the third trimester, the mother’s bones must get damaged.
Researchers are trying to determine how/when this damage occurs, where the damage occurs, does calcium supplementation help this process, and whether the damage is temporary or increases the mother’s long term risks for osteoporosis.

However, it is possible that pregnant women’s bodies adapt to increased calcium requirements. Some studies indicate that even if bone loss occurs, it is temporary and reversed approximately 6 to 12 months after weaning, ultimately resulting in no major effect to bones (even without calcium supplementation).
Women may be able to improve postpartum bone loss recovery through exercise. An animal study published in June 2021 determined that postpartum weight-bearing exercise appears to initiate higher bone recovery, especially during lactation.
Women should read more information about calcium requirements during pregnancy.
Action
Pain in the pelvic region, back, and/or joints should always be assessed by an HCP, and women should not feel they need to wait until the next scheduled appointment to mention it if symptoms are too distressing or debilitating.
While physical activity is also important during pregnancy, it needs to be smart; women need adequate rest and recovery periods. Women also need to avoid any activity or prolonged activity that could cause potential injury leading to chronic pain or even disability in the postpartum period.
Acetaminophen (Tylenol®) is often the first-line recommended medication for joint and back pain during pregnancy, and is considered safe when used appropriately.
Partner/Support
Joint pain is real during pregnancy and can be debilitating for some women. If a pregnant woman overuses her joints, or does any activity for a prolonged period that puts additional strain on her joints, she could risk potential injury that could cause chronic pain or even disability in the postpartum period.
Since exercise is also important during pregnancy, the woman's partner can help her engage in light to moderate physical activity with adequate recovery and hydration, and stopping at any point she feels pain. Engaging in activities together can make walking/hiking more enjoyable, and allows the partner to be there in case the woman experiences any injury/pain.
Resources
Preventing Falls (American Orthopaedic Association; although the article focuses on the elderly, the advice/recommendations are completely applicable to pregnant women)
Pelvic Pain in Pregnancy (U.K. National Health Service)
Pelvic Partnership (Online Support Group)
Pelvic Girdle Pain Information Booklet (Pelvic Obstetric and Gynaecological Physiotherapy)