Calcium

While calcium is necessary during pregnancy to protect both the mother’s bones and the fetus’ skeletal development, research does not appear to indicate that routine supplementation is required during pregnancy unless a woman is considered deficient.
Research has indicated that any bone loss in the mother as a direct result of pregnancy rapidly reverses around 6 to 12 months postpartum, even with shortly spaced pregnancies. Therefore, current daily recommendations for calcium during pregnancy are the same as non-pregnant women.
Pregnant women who consume dairy products through a varied diet are likely receiving an adequate amount of calcium. Women who do not consume dairy products should talk to their health care providers (HCP) if they are concerned about their calcium status. Calcium can also be obtained through more targeted plant sources or supplements when recommended by an HCP.
Background
Calcium is the most abundant mineral in the body, essential for bone formation, muscle contraction, and enzyme and hormone functioning; 98% of the body’s calcium is found in the bones and teeth.
It is estimated more than 50% of women in the United States do not get enough calcium. Calcium intake is especially crucial during pregnancy and lactation because of the potential negative effects on maternal bone health if maternal calcium stores are depleted.
Inadequate consumption of calcium during pregnancy can lead to weak bones, tremor, tingling or numbness, muscle cramping and tetanus. The fetus can experience delayed growth, low birth weight, and poor bone mineralization.
Pregnancy
The fetus accumulates about 30 grams (g) of calcium over the course of pregnancy. Newborns have the highest levels of calcium in their bodies compared to children and adults.
Ossification of fetal limb bones begins around 10 weeks of pregnancy and starts to make demands on the mother’s supply of calcium.
Compared to pre-pregnancy, pregnant women's absorption of calcium almost doubles as early as 12 weeks, which appears to be the major maternal adaptation to meet the fetal need for calcium.
Calcium absorption in a woman who is not pregnant is estimated to be 35%; in a pregnant woman in her third trimester, calcium absorption is increased to an estimated 60%.
The average calcium transfer to the fetus during pregnancy is 50 milligrams (mg)/day during the second trimester and up to 330 mg/day during the third trimester (1,000 mg = 1 gram).
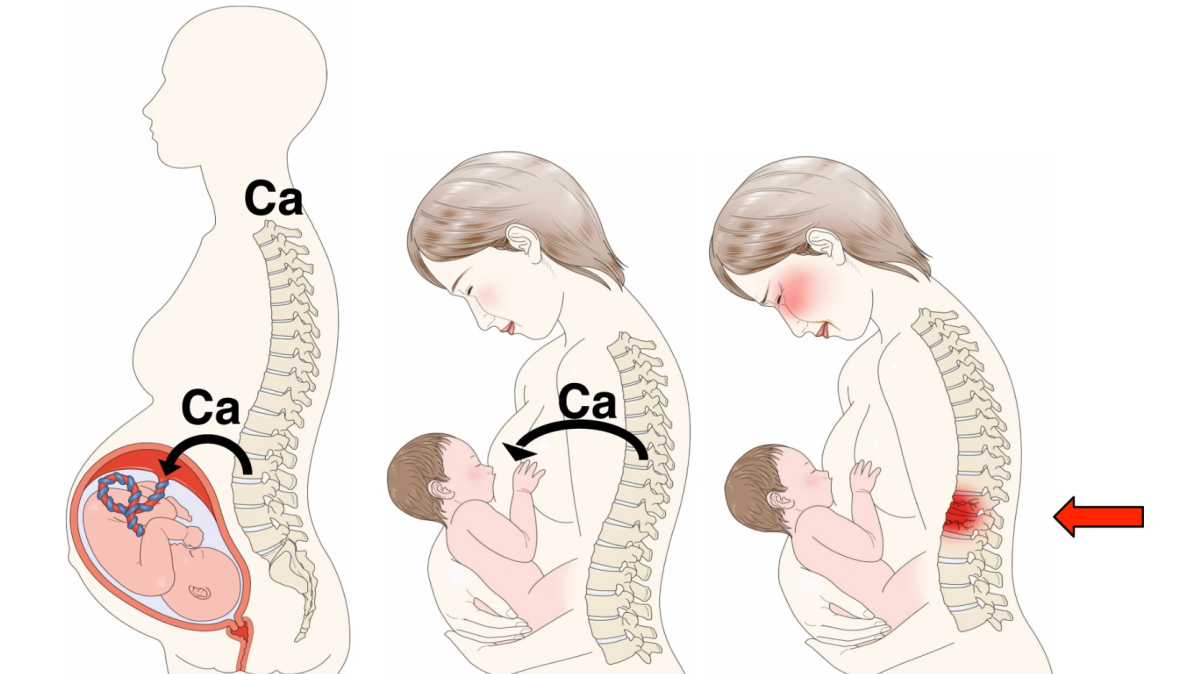
The biggest concern regarding a lack of calcium during pregnancy is the potential damage to the mother’s bones, since the fetus takes calcium from the mother’s skeleton if there is not enough in the mother’s diet.
It is theorized that because the calcium transfer is so fast and so intense in the third trimester, the mother’s bones must get damaged. Researchers are trying to determine how this damage occurs, where the damage occurs, does calcium supplementation help this process, and whether the damage is temporary, or increases the mother’s long term risks for osteoporosis.
Research Regarding Supplementation
Because the above questions have not been completely answered, recommendations for calcium during pregnancy and lactation vary around the world.
Advocates for calcium supplementation during pregnancy indicate calcium can be directly linked to increased bone density and bone length of newborns, and that supplementation can reduce a mother’s bone loss during pregnancy.
However, it is possible that pregnant women’s bodies physiologically adapt to increased calcium needs as other studies indicate that even if bone loss occurs, it is temporary and reversed after weaning, ultimately resulting in no major effect to bones.
Further, the complete recovery of bone occurs in most women, even with shortly spaced pregnancies, which is likely aided by the resumption of menstruation.
Even though breastfeeding can further deteriorate bone density in the mother (an additional 5% to 10%), additional calcium intake does not appear to prevent bone loss during lactation either, as any loss has been documented to rapidly recover approximately 6 to 12 months after weaning, in most cases.
There does not appear to be enough strong evidence to routinely recommend calcium supplements to pregnant women who get enough calcium in their diet. Pregnant women who eat diets with low calcium content will likely benefit much more from a calcium supplement, since they are entering pregnancy with an already depleted skeleton.
Some studies have linked calcium supplementation with a lower risk of preeclampsia and high blood pressure risk, but it is possible those women were already deficient.
Further, the calcium requirement for the fetus is met mainly by increases in the mother’s calcium absorption and the way her body uses calcium in her bones. Calcium supplementation could theoretically interfere with the mother’s ability to conserve calcium on its own during pregnancy.
A systematic review and meta-analysis of seven randomized controlled trials published in November 2021 concluded "no advantage of calcium supplementation was found on maternal bone mass density after delivery or during breastfeeding, even when dietary calcium intake was low." Further, a suspicion of some long-term harm of possible supplementation on bone mass density was raised based on the data. The study concluded "the impact of calcium supplementation on maternal and offspring bone health was deemed unknown because of inconclusive research results."

There is some research regarding calcium supplementation and the prevention of cavities (caries) in children as they grow up. Primary tooth formation and mineralization starts during fetal development, and higher intakes of dairy products by the mother have been linked to better cavity prevention in those children.
However, other studies indicate that neither calcium nor fluoride supplementation is necessary for this outcome as long as children have access to fluoridated dental products such as toothpaste and mouthwash when their teeth come in.
Recommendations
Most international health organizations for pregnant and lactating women recommend approximately 1,000 mg/day, the same as non-pregnant women. The average consumption of calcium in pregnant women is around 800 mg/day.
The World Health Organization recommends 1,500 mg to 2,000 mg daily for pregnant women with low dietary calcium intake, such as those who avoid milk products or are on certain medications.
For women carrying multiples, some experts recommend up to 2,000 to 2,500mg/d of calcium and 1,000 IU of Vitamin D daily.
Vitamin D and calcium should be taken together and are usually formulated together in supplements. Vitamin D can double the absorption rate of calcium, and deficiency in either could lead to more severe skeletal depletion.
Overall, calcium supplementation is safe during pregnancy. However, it is possible to take too much, which leads to a condition known as hypercalcemia. Hypercalcemia can cause constipation, nausea, vomiting, kidney stones, bone pain, fatigue, and confusion. The upper daily limit for calcium in pregnant women has been established at 2,500 mg/day, the same for non-pregnant women.
Many pregnant women use antacids during pregnancy for heartburn, which contain calcium in the form of calcium carbonate and calcium citrate.
Pregnant women should not use or take heartburn tablets to obtain extra calcium; however, women who do take them for symptom control can use the tablets toward a daily calcium requirement.
Antacids are considered safe during pregnancy (See Heartburn/Acid Reflux).
Note: Although routine calcium supplementation is not recommended during pregnancy (such as folic acid), obtaining enough of the nutrient is still very important.
Food Sources
The main dietary sources of calcium are milk, dairy products, calcium-set tofu, leafy greens (kale), almonds, broccoli, edamame, chickpeas, pinto beans, spinach, and fortified foods and juices. Pregnant women should look for almond milks that are fortified with calcium if they prefer to avoid cow’s milk.
Interestingly, the ability to digest lactose may improve for some women during pregnancy, especially later in pregnancy. Pregnant women may be able to drink milk and eat other dairy products without discomfort as they progress through pregnancy (specific to intolerance only, not allergies).

Action
Women who are concerned about their calcium intake or have questions should have a discussion with their HCP regarding possible calcium supplementation. Calcium levels are normally checked at the first prenatal appointment through a blood test that will also provide other nutrient values.
Women should never take any supplements during pregnancy without talking to their HCP first.
Resources
Calcium and Vitamin D (National Osteoporosis Foundation)
Calcium Fact Sheet (U.S. National Institutes of Health)