Lungs (Respiratory System)

Pregnancy causes unique changes to the respiratory system. The rib cage spreads up and out, the diaphragm is pushed up, muscle strength is reduced, and women can feel out of breath from normal everyday activities.
These changes are due to the extra oxygen requirements during pregnancy and the enlarged uterus putting pressure on the rib cage and diaphragm. Women can feel as if they are short of breath or breathing too fast.
Fortunately, as the baby drops near term, the top of the uterus lowers, and the respiratory system gets a bit of relief, with almost full and immediately resolution after delivery.
Respiratory symptoms can be normal during pregnancy, but must always be brought to the attention of a health care provider (HCP) to rule out other causes. For example, shortness of breath is both a normal symptom of pregnancy as well as a "first sign/red flag" symptom for other more serious (but uncommon) concerns. HCPs will want to evaluate women for these possible complications, conditions, or infections.
Women should read more below to learn why breathing can feel difficult during pregnancy, why their bra strap size has changed, and when they can feel like they can breathe normally again.
Background
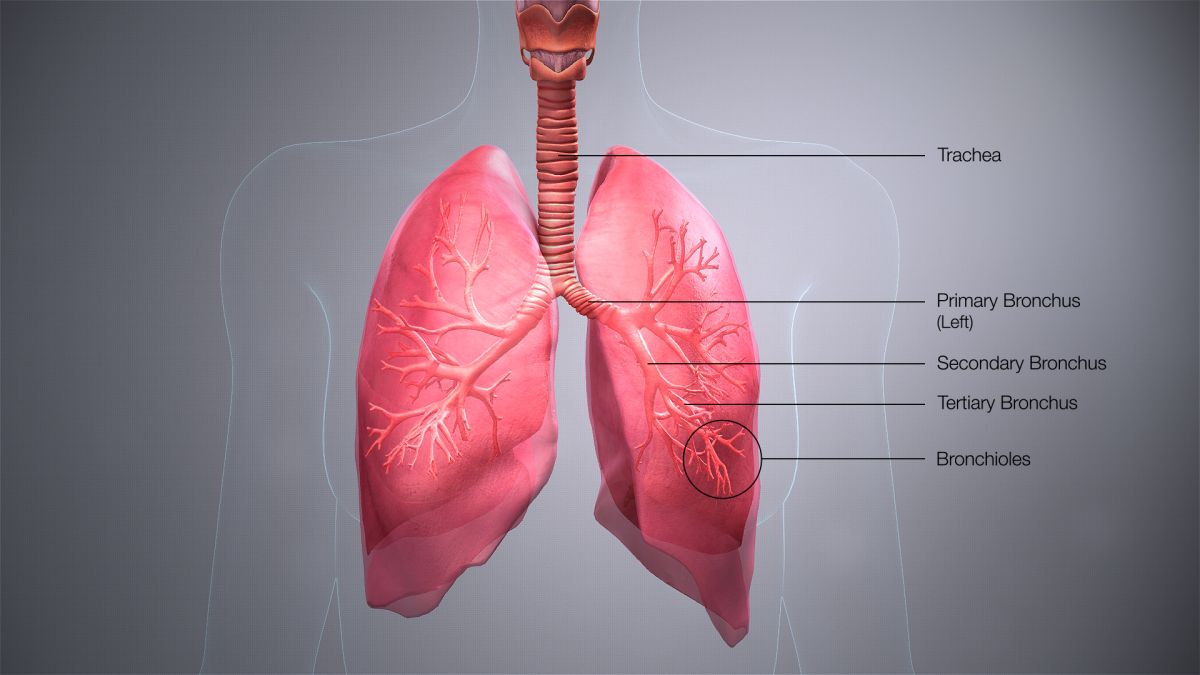
Many changes occur in the respiratory system during pregnancy; this system includes the nose, pharynx, larynx, trachea, bronchi, and lungs.
As a result of these changes, pregnant women may experience signs/symptoms such as shortness of breath, fatigue, a larger rib cage, and a change in bra band size.
These changes are also theorized to increase the risk a pregnant women may experience severe respiratory illness (i.e. influenza).
Diaphragm and Rib Cage
Additional factors include breast enlargement, weight gain, fluid accumulation, and easier spreading of the ribs due to loosening of the ligaments.
The chest increases in circumference by 5 to 15 centimeters (cm) during pregnancy (not including breast size). Flaring of the ribs begins at the end of the first trimester, which is when the lower part of the rib cage juts forward slightly. Spreading of the ribs may cause some women to notice their bra strap size needs to increase, rather than just the cup size.
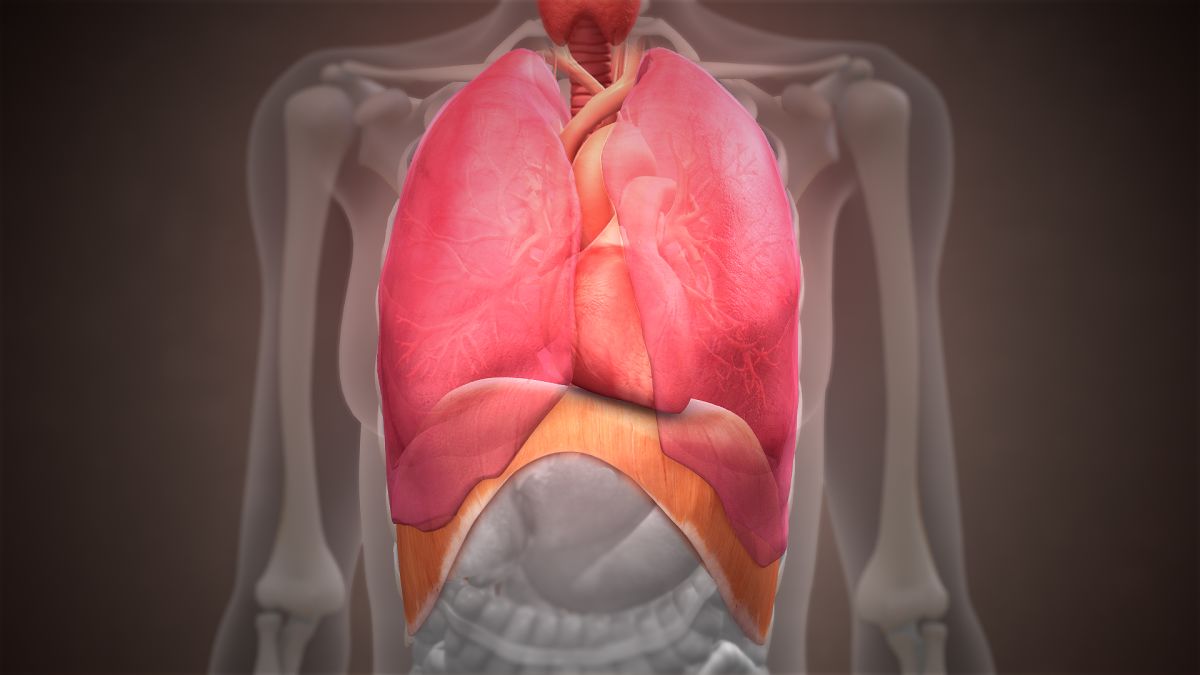
The diaphragm is a dome-shaped structure of tendon and muscle that is very thin (2 to 4 millimeters) and concave on its lower side; it separates the chest from the abdomen. It is important for posture and for proper organ function and placement. It also provides the structure necessary for breathing. Therefore, when this structure moves (as in pregnancy), breathing can be affected.
Breathing
Upward pressure of the uterus and diaphragm causes two things to happen: reduction of expiratory reserve volume (ERV) and reduction of functional residual capacity (FRC).
ERV: The amount of air an individual can forcefully expel after exhaling normally. (Imagine taking a normal breath out, and then forcing all additional air out as much as possible, contracting the muscles/diaphragm).
FRC: The amount of air left in the lungs after a normal exhalation, that includes what can be expelled (ERV) and what an individual cannot expel, known as Residual Volume (RV). Therefore, FRC = RV + ERV.
Extra air remaining in the lungs after exhalation is essential, as this extra air helps keep the small airways open. This volume of air is what is decreased during pregnancy, but not completely.
FRC decreases by approximately 20% to 30%, or 400 to 700 milliliters (ml) during pregnancy (normal total volume is 2,400 ml). This lowers the overall oxygen reserve a woman has, and with an increased amount of oxygen needed during pregnancy, can cause feelings of shortness of breath, or breathing faster.
However, even with discomfort, pregnant women still get enough oxygen, even though it may not feel like it. Women should always report any breathing difficulties to their HCP.
The diaphragm can rise by as much 5 cm as the uterus grows, and women can feel like it is more difficult to breathe later in pregnancy, especially when sleeping.
Fortunately, women do catch a small break very close to term. At 36 weeks, the fundal height (top of the uterus) is about two inches below the xiphoid process (sternum); but at 40 weeks, it is four inches below. This is due to engagement and descent of the baby’s head, which lowers fundal height. This is the “drop” that most women report, and usually results in easier breathing.

Shortness of breath, which results in women breathing very fast until they can “catch their breath”, is reported by up to 70% of healthy pregnant women during normal daily activities, starting very early in pregnancy. The experience of this symptom in the first trimester points to hormones playing a significant role at this time, since the uterus and other lung/chest changes have not yet occurred.
It is believed that the rise of progesterone in early pregnancy may be the cause, but this is debated. Further, some researchers believe that respiratory rate is unchanged during pregnancy, and that pregnant women do not breathe any faster than women who are not pregnant.
However, other research indicates pregnancy is associated with “over breathing”, or an increase in the amount of air a woman breathes in and out, with most of the change occurring in the first trimester.
It is possible this conflict arises from women adapting differently to the hormonal and physical changes of pregnancy. The overall pulmonary and cardiac health of the pregnant woman likely also plays a role.
Multiples
Respiratory changes in pregnancies with multiples are also debated. Some researchers believe all changes described above are further increased for multiples in comparison to single babies, while others believe there are no additional differences.
However, women carrying multiples can be more fatigued, require more energy output, and experience greater cardiac changes. Together, these changes can make women pregnant with multiples feel more "severe" respiratory discomfort.
Postpartum
Most of the physical respiratory changes described above return to normal after delivery. The diaphragm almost immediately moves back down as the uterus lowers to the level of the belly button.
Other changes, especially those that may remain as breastfeeding begins (breast weight, rib spreading), could take up to six months to return to normal.
Action
Women need to report all respiratory symptoms to their HCP immediately. Although shortness of breath is common, it is a known challenging symptom for women to experience and for HCPs to assess, as it can be a "first sign/red flag" symptom for other more serious concerns during pregnancy, to include cardiac issues (although these are not common), venous thrombolytic events, or respiratory infections.
HCPs can also help women manage this symptom, especially when other concerns have been ruled out.
Partner/Support
Shortness of breath is a scary symptom for women to experience, and partners may often not know how to help or how best to react.
Although this symptom is considered normal the vast majority of the time during pregnancy, partners can play an important role in helping women recognize possible warning signs. Read Shortness of Breath for more information.
Resources
Respiratory System Anatomy (Canadian Lung Association)