Obesity

While obesity during pregnancy is increasing world-wide and includes greater risks of complications for both the woman and her baby, women considered "obese" can still experience perfectly healthy pregnancies.
Research indicates that pre-pregnancy weight may be a larger factor for potential problems than total amount of weight gained during pregnancy; therefore, women should aim to be as healthy as possible before conception.
Although numerous conflicting and confusing guidelines exist regarding the management of obesity during pregnancy, the overarching recommendations appear to be that women should aim for as much nutrition as possible with each meal, engage in regular physical activity (even walking), and enjoy favorite foods in moderation.
For women who are currently considered obese but trying to conceive, it has been shown that losing just 5% to 10% of their current body weight may have dramatic positive effects on pregnancy outcome.
Women should talk to their HCP regarding their weight prior to and during pregnancy if they have any questions or concerns. Women can also read Weight and Nutrition to learn more.
Background
"Obese" and "obesity" are clinical terms applied in research and in a clinical setting as a specific condition; as such, we use these terms only for consistency (for example, rather than "plus-size").
Being overweight or obese prior to pregnancy are both associated with a variety of complications and are considered two of the most common health risks during pregnancy. Obesity has the highest prevalence among metabolic disease in pregnancy and has doubled in the last 20 years, leading to an increase in adverse outcomes for both mother and baby.
In Western countries, the prevalence of obesity in pregnant women has strongly increased, with reported prevalence rates reaching 30%; further, an estimated 40% of women gain more weight than recommended during pregnancy (based on pre-pregnancy Body Mass Index (BMI)).
Obesity is a term that indicates a woman has a weight significantly higher than is recommended to avoid problems. Definitions of "normal-weight", "overweight" and "obese" have been defined; however, new terms are used to describe more severe degrees of obesity.
According to the U.S. Centers for Disease Control and Prevention:
If BMI is less than 18.5, it falls within the underweight range
BMI is 18.5 to < 25, it falls within the normal range
BMI is 25.0 to < 30, it falls within the overweight range
BMI is 30.0 or higher, it falls within the obese range

Obesity is further subdivided into categories:
Class 1: BMI of 30 to < 35
Class 2: BMI of 35 to < 40
Class 3: BMI of 40 or higher; Class 3 obesity is sometimes categorized as “extreme” or “severe” obesity.
Note: BMI is a screening tool based on calculating weight and height; however, it does not take muscle mass or fitness into account and is not a perfect index tool. An HCP needs to complete a physical exam for a better assessment of overall health.
Despite these classifications, guidelines regarding obesity during pregnancy, to include weight gain recommendations, nutritional plans, and the prevention of potentially associated pregnancy complications are inconsistent and can be confusing. Further, our understanding of the long-term effects of obesity before/during pregnancy on infant outcomes is limited.
How Obesity Affects Pregnancy Outcomes
When researchers find a potential association between an adverse outcome (e.g. large birth weight) and obesity, they then try to determine the mechanism of action – "how" obesity can cause that complication.
Current mechanisms for how/why being overweight can cause certain complications during pregnancy:
Insulin Resistance: Insulin resistance is a normal occurrence during pregnancy, but women who are considered obese may have more severe resistance, which may lead to gestational diabetes and/or large birth weight. Insulin resistance = more glucose in the mother's blood. This glucose is transported across the placenta to the fetus, which causes large weight gain.
Lipid Metabolism: Pregnancy-related insulin resistance affects lipid metabolism; this can increase triglyceride and cholesterol levels late in pregnancy. In obese pregnancies, this means the fetus is exposed to high levels of free fatty acids throughout all stages of gestation. In turn, this promotes inflammation. It is this excess inflammation that can lead to complications (e.g. placental concerns and high blood pressure/preeclampsia).

Associated Short-Term Complications
Pre-pregnancy obesity may pose a greater risk of complications that women who simply gain too much weight during pregnancy, but started pregnancy at a healthy weight.
Women who are considered obese prior to pregnancy have more risk for gestational hypertension, micronutrient deficiency, gestational diabetes, birth defects, higher birth weight, assisted delivery, induction of labor, and cesarean delivery than women who gain too much weight during pregnancy.
Note: Risks associated with obesity during pregnancy does not mean these risks will always occur, only that increased risk exists.
Potential complications include:
Fertility: Obesity is linked to an abnormal follicular environment and smaller oocytes that may be less likely to fertilize or implant normally, especially in the setting of in vitro fertilization.
However, it has been reported that even a moderate decrease of less than 10% in preconception weight improves maternal health and obstetrical outcomes.
Miscarriage: Although debated, higher rates of miscarriage have been associated with obesity; these results have led to the recommendation that women who are trying to conceive or have a history of miscarriage (especially recurrent) may have better success with a reduction of their BMI.
Obstructed Sleep Apnea (OSA): HCPs may screen for OSA during pregnancy; OSA is characterized by episodes of nocturnal apnea (shallow or paused breathing), interrupted sleep, and variable degrees of airway obstruction.
Gestational Diabetes: Gestational diabetes is a condition during pregnancy in which the pancreas does not produce enough insulin and glucose builds up in the blood; risk may be four times greater than women of normal weight.
Large birth weight: Pregnant women considered obese may be at risk of delivering a large baby for gestational age, known as macrosomia; the risk is further increased if the woman also has gestational diabetes; both can lead to cesarean delivery.
Cesarean delivery and wound infection: Increased weight during pregnancy has been associated with a higher risk of cesarean delivery (overall) as well as wound infection.
Gestational Hypertension: High blood pressure during pregnancy is a “flag” and potential precursor to preeclampsia; gestational hypertension occurs when a woman who previously had normal blood pressure develops high blood pressure when she is more than 20 weeks pregnant (but has no protein in her urine); approximately 25% of women with gestational hypertension go on to develop preeclampsia.
Preeclampsia: Women who are obese during pregnancy also have a higher risk of developing preeclampsia; preeclampsia is a pregnancy-specific, serious vascular disorder affecting both mother and baby, and virtually every organ system in the mother.
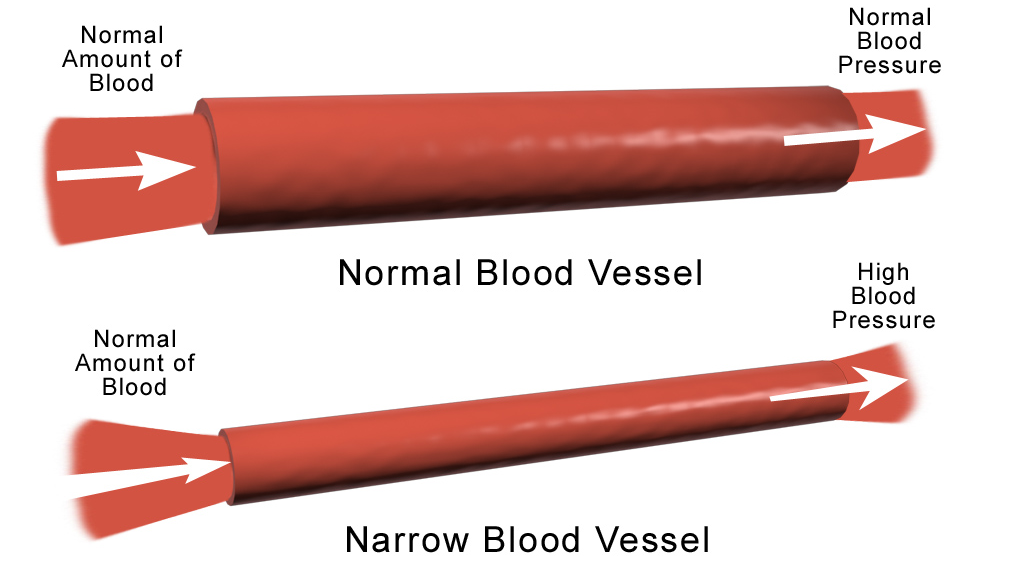
There is a strong association of increased preeclampsia risk and obesity during pregnancy. Although the mechanisms whereby obesity increases this risk are not known, and not all obese women develop preeclampsia. However, inflammation may be a primary driver, along with blood vessel development.
Preeclampsia begins as a vascular disorder (blood vessels) within trophoblastic cells that create the placenta and promote oxygen exchange between the mother and fetus. Very early in pregnancy, these cells help to remodel the uterine spiral arteries so these arteries can supply nutrients and blood to the placenta/fetus.
Endometrial and spiral artery blood flow is reduced in obese women before pregnancy, which could lead to a further reduction of blood flow during pregnancy. Additionally, obese women may experience improper blood vessel development within the placenta, leading to complications.
A failure of the remodeling and development of these arteries in the uterus and placenta results in a restriction of blood supply because the connection between mother and placenta is inadequate – the arteries fail to anchor deeply enough.
Obesity and late-onset preeclampsia are also associated with larger fetal growth, larger birth weight, and a heavier placenta. A heavier than normal placenta is associated with a lack of oxygen to the fetus. It is known that the number of capillaries in the placenta is increased in obesity, and these blood vessels may become too constrained near term, cutting off oxygen supply.
Postpartum: Obesity is associated with possible complications in the postpartum period, to include venous thromboembolism, depression, and difficulty breastfeeding.
Possible Long-Term Complications
Recent studies indicate that placental function plays a critical role in the long-term health of the baby, known as fetal programming; this is considered “newer” research so the exact mechanisms for how this may occur have not yet been established.
Obesity is currently a condition associated with fetal programming. Fetal programming (“Barker hypothesis”) occurs when the normal fetal development is disrupted by an outside influence applied to a critical point during gestation that affects the baby for this rest of his/her adult life.
For example, the mother’s diet can influence the newborn’s body composition, metabolism, and nutritional habits later in life, likely due to the type and amount of nutrient transport through the placenta (occurs with both under- and overnutrition).

Management
Various researchers have documented approximately 26 national and international guidelines associated with different aspects of the management of obesity in pregnancy.
Although very inconsistent, the overarching goal of these guidelines is reach the point in pregnancy in which the baby can be born healthy with the least amount of complications for both mother and baby.
Women should aim for the healthiest BMI possible prior to conception; it has been demonstrated that delaying conception until the BMI reaches recommended levels seems to dramatically improve pregnancy outcomes – even 5% to 10% weight loss can have a dramatic positive effect.
Although research has shown weight loss should theoretically decrease these risks, research regarding weight loss during pregnancy and its associated outcomes is understudied and data is limited.
Therefore, weight loss is not recommended during pregnancy, but can improve outcomes prior to pregnancy. However, women may be asked to minimize their weight gain.
Weight gain recommendations:
BMI 25 to 29.9 (overweight): 15 to 25 pounds (7 – 11.5 kg)
BMI 30 or more (obese): 11 to 20 pounds (5-9 kg)
Read more on weight.
Action
It is often recommended women have a preconception appointment with their HCP to get any medical conditions or precursors under control prior to pregnancy to increase the chances for a healthy, full-term pregnancy.
Women should aim for the most nutrition possible in each meal and stay within healthy caloric recommendations, but also enjoy favorite foods in moderation.
Women should also accompany a healthy diet with regular physical activity during pregnancy, even if this only includes walking. Physical exercise has enormous benefits during pregnancy and may reduce the risks of complications. Read more.
For women who are currently considered obese but trying to conceive, it has been shown that losing just 5% to 10% of their current body weight may have dramatic positive effects on pregnancy outcome.
Women should talk to their HCP regarding their weight prior to and during pregnancy if they have any questions or concerns. Women can also read Weight and Nutrition to learn more.
Women should also consider sharing and submitting their experience below regarding being considered obese while pregnant (or trying to get pregnant). This can help other women learn additional perspectives about weight during pregnancy.
Partners/Support
Partners can help women during their pregnancy by aiming to eat healthier themselves, in an effort to support the woman in her own eating and exercise habits. Couples who strive to eat healthier, make smarter choices, and engage in more physical activity together, are more likely to be successful.
Resources
Calculate BMI here.
National Child and Maternal Health Education Program - Pregnancy for Every Body.