Causes of Pregnancy Loss

Pregnancy loss is devastating, and the inability to determine a cause can compound feelings of considerable guilt and frustration.
The "cause" of miscarriage is now considered multifactorial – meaning that it is more than likely multiple forces act at the same to cause pregnancy loss, most of which are completely out of a couples’ control.
While the vast majority of causes cannot be identified, some are easily diagnosed, and treatments are straightforward and effective. However, other causal factors may be more complicated, so the best recommendation based on current knowledge is for couples to seek preconception appointments that also includes genetic counseling – prior to becoming pregnant.
Women should not hesitate to ask their health care provider (HCP) about possible causes or screening tests. Although medicine does not have all the answers regarding human reproduction, in many cases, HCPs can provide women with more information and potential answers so women can make better informed decisions regarding their own reproductive health.
Further, many women who experience even multiple miscarriages go on to have healthy, full-term pregnancies in the future.
Background
Early pregnancy loss can have a significant psychological toll on affected couples, and some couples will lose more than one pregnancy. Research is aiming to identify the causes of miscarriage, improve treatments, and decrease the time needed for a successful pregnancy.
However, determining why so many early pregnancies fail is very difficult, despite how often it occurs. Further, it is currently assessed that most miscarriages are likely multifactorial – with more than one causal factor acting at the same time (i.e. chromosomal abnormalities, environmental triggers).
It is recommended, if possible, that couples have preconception appointments. This appointment could potentially a catch a treatable condition that can be successfully managed prior to trying to conceive.
For example, hormonal disorders, diabetes, thyroid dysfunction, fibroids, and anatomic anomalies are spotted and corrected easily and have high degrees of success for future pregnancy.
Women/couples should also understand there is no specific time frame couples must “try” before asking for medical help. Most HCPs find it appropriate to evaluate a couple for potential concerns after two consecutive losses, regardless of the time frame.
HCPs will ask questions regarding both partners’ medical histories as well as the woman’s reproductive history including previous pregnancies and miscarriages – similar to a preconception appointment.

HCPs will try to assess what could potentially be causing pregnancy loss and attempt to identify a possible treatment. This process is imperfect, requires a lot of trial-and-error, and can take time.
HCPs may also refer women/couples to a genetic counselor or reproductive endocrinologist, and recommend various support groups that can help women/couples remain hopeful, understand this process better, and recognize they are not alone.
Chromosomal Abnormalities
Of the known causes of miscarriage, chromosome abnormalities are the most common. The prevalence of chromosomal abnormalities in women with a single miscarriage may be as high as 80%.
Endometrial cells that have prepared for pregnancy (decidualized) appear capable of specifically selecting embryos for implantation on the basis of their quality. It is possible that some women (especially in recurrent miscarriage) may be allowing embryos of poor viability to implant.
A parental chromosomal anomaly is found ten times more frequently in couples experiencing recurrent miscarriage than in the background population.
“Advanced” maternal age is also a strong risk factor for miscarriage. The number of good quality oocytes in older mothers is fewer than younger mothers, which increases the frequency of chromosomal abnormalities leading to miscarriage. However, extensive research has recently begun to challenge this notion.
In vitro fertilization (IVF) plus prenatal genetic testing is a recommended strategy in the management of chromosomal abnormalities, as IVF improves sperm and egg quality and increases the chances of a higher quality embryo implanting successfully.

Bleeding
Although bleeding is a very common symptom of miscarriage, it is not clear if bleeding itself can cause miscarriage, as bleeding prior to a miscarriage has not been well studied. Further, bleeding early in pregnancy does not mean a miscarriage will always occur (read Vaginal Bleeding for more detailed information).
Hormones – General
The luteal phase is the period between ovulation and either the onset of pregnancy or the start of menstruation. During this time, progesterone is secreted by the corpus luteum to thicken the endometrial lining in anticipation of implantation. If implantation does not occur (no HCG), then the corpus luteum dies, progesterone lowers, and menstruation begins.
Luteal Phase Insufficiency (LTI) (formerly luteal phase defect or deficiency) is controversial. Traditionally, LPI was proposed to result from inadequate production of progesterone by the corpus luteum, and women suspected of having this condition were prescribed progesterone from approximately four to ten weeks of pregnancy. It is theorized that conditions such as polycystic ovaries and thyroid and prolactin disorders may also by themselves cause LPI.
The controversy stems from some research that shows progesterone is not effective for the reduction of miscarriage in women suspected of having LPI. However, there is no reliable method for diagnosis of progesterone deficiency during luteal phase or early pregnancy, therefore it is possible that not all women diagnosed with LPI truly have the condition (and therefore, supplemental progesterone would not work for these women).
Blood tests to measure progesterone levels are not valuable as there is a wide range of “normal”, no minimum required amount has been established to indicate deficiency, and levels of progesterone in early pregnancy are constantly in flux (blood levels range from 2 to 40 ng/ml).
In general, a review published in April 2021 indicated the overall available evidence suggests that progestogens probably make little or no difference to live birth rate for women with threatened or recurrent miscarriage. Vaginal micronized progesterone may increase the live birth rate for women who are experiencing early pregnancy bleeding and have a history of one or more previous miscarriages, with likely no difference in adverse events.
Regardless, there is no doubt that progesterone supplementation has been successful in many cases, but the full effectiveness, dose, and length of time necessary is still debated. Most importantly, there is currently no evidence that progesterone supplementation harms a fetus, and therefore it is assessed there is very little risk in attempting this treatment.
It is also possible the trophoblast could produce too little HCG which then lowers progesterone levels resulting in miscarriage. It is therefore theoretically possible that HCG injections could assist, but this has not been well studied in comparison to progesterone supplementation. Currently, HCG is most often used to boost fertility rather than to maintain a pregnancy.
Poorly controlled type 1 diabetes is another hormone-associated condition that could cause pregnancy loss. Type 1 diabetes occurs when the pancreas does not make insulin (a hormone) to breakdown sugar (glucose) in the bloodstream; therefore, cells cannot use the glucose for energy.
Thyroid Hormones
Thyroid disorders, especially hypothyroidism, have long been associated with infertility, and many researchers advise routine thyroid hormone testing in all pregnant women – ideally, before pregnancy.
Hypothyroidism is assessed to be the second most common hormonal disorder diagnosed during pregnancy – after diabetes. The prevalence of pregnant women with hypothyroidism could be as high as 3%. However, it is likely this number is higher as evaluating women for this condition is not yet routine in all obstetric practices.
Thyroid hormones:
T3: Triiodothyronine (contains 3 atoms of iodine)
T4: Thyroxine (contains 4 atoms of iodine)
TSH: Thyroid stimulation hormone
Inadequate amounts of thyroid hormones can cause miscarriage. Low amounts of these hormones can also cause problems with fetal growth and development, especially the central nervous system. Routine screening for these hormones is advised due to these concerns and because the condition is easily treated.

Production of T4 increases by approximately 50% to 100% during pregnancy and the embryo/fetus relies solely on the mother’s thyroid hormones the entire first 20 weeks.
Further, receptors for thyroid hormones are present in the fetal brain from 8 to 9 weeks of pregnancy, but the fetus doe not make any thyroid hormone until the second half of pregnancy. It is therefore critical this condition is diagnosed prior to, or very early in pregnancy.
Routine testing for these hormones prior to pregnancy is especially important as most women may not have any symptoms related to low levels (asymptomatic hypothyroidism). For women who do present with symptoms, these include weight gain, feeling cold, dry skin, constipation, fatigue, and drowsiness. Some of these symptoms can be easily mistaken for pregnancy-related symptoms.
While there is lack of consensus regarding the definition of what should be considered the normal upper limit of TSH before/during pregnancy, the leading cut-off value appears to be a TSH value more than 2.5 mIU/L. Therefore, the aim of treatment is to maintain a baseline of under 2.5 mU/L.
Hypothyroidism is treated with levothyroxine (small tablet). Women who take the medication prior to pregnancy may need to increase their dose by as much as 50% during pregnancy. Hormone levels are usually checked every for to six weeks to make sure the medication dosage does not need to be increased.
Subclinical (borderline) hypothyroidism occurs when TSH levels are just above normal. Although impacts to the fetus when the mother has subclinical hypothyroidism is not as well known, adverse effects could be subtle, but research is inconsistent. A woman's HCP will determine if treatment may be necessary in these cases.
Uterine and Cervical Abnormalities
Physical structures of the uterus can impede the ability to get pregnant, and include congenital uterine anomalies, adhesions, fibroids, and polyps.
Congenital abnormalities are the consequence of an abnormal development of the Müllerian ducts and include septate, bicornuate, unicornuate, didelphic, and arcuate uteri. They are reportedly found in up to 10% of women with recurrent pregnancy loss.
Although having any of the above abnormalities during pregnancy can raise the risk of miscarriage, pregnancy is still possible without surgery. However, surgical correction (fibroids and uterine structural concerns) also has a high success rate for future pregnancies.
Cervical Insufficiency is a common cervical cause of miscarriage and preterm labor. The cervix is the opening to the uterus that sits at the top of the inside of the vagina and has an opening at each end; these openings are blocked (mucus plug) during pregnancy.
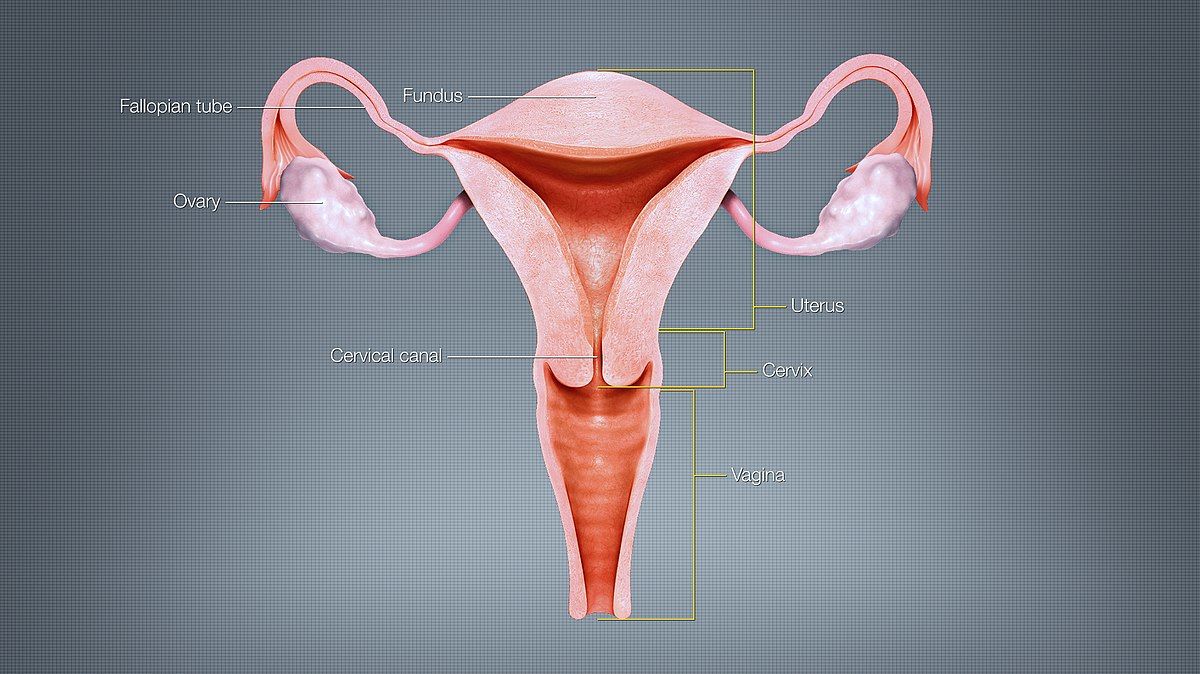
Cervical insufficiency (previously incompetent cervix) is usually defined as a “mechanical” or tissue failure of the cervix that leads to painless premature softening, shortening, and dilation – usually without contractions – that may result in preterm delivery or loss of a pregnancy (read Insufficient Cervix).
Immune System
The body’s response to the implantation of the blastocyst is poorly understood, but current research indicates a woman's immune system creates a necessary inflammatory response that assists in successful implantation. As more research is completed, and the inflammatory response necessary for implantation is more thoroughly understood, additional treatments can become available.
Previously, the leading hypothesis was that the mother’s immune system must be significantly suppressed in order to allow pregnancy to occur – but instead, the immune system is quite active.
It is now believed the significant presence of the woman’s immune cells at the implantation site that surround the trophoblast (i.e. an inflammatory reaction), is not a response to a “foreign invader” as previously believed, but a response to assist in its growth and development.
Therefore, the mother’s immune system is not only quite active at the implantation site, but its high activity is necessary for successful implantation. It is theorized that the fetal/placental unit also has its own immune system, which works together with the woman’s, instead of against it.
This is further evidenced by the negative effects that occur due to removal of immune cells at the implantation site. When these cells are removed, trophoblast cells cannot reach deep into the uterine wall and implantation is unsuccessful. The observed inflammation is a necessary component, not the body trying to reject it.
A properly regulated immune system is therefore necessary in early pregnancy. There is also some evidence that an overactive immune system could also interfere with implantation and cause pregnancy loss. A study published in May 2021 showed that the decidua (uterine lining) of women with recurrent miscarriage expressed almost 51-times higher values of the cytokine IL-7 (component of the immune system) in gene expression analysis (future treatment may be possible).
Uterine natural killer (uNK) cells are the most abundant immune cell population in endometrium, constituting up to 80% of lymphocytes (white blood cells) in uterine decidua in early pregnancy.
Despite their name, they do not harm the embryo; they prepare the endometrium for implantation and may also help promote placental development.
Their role in miscarriage is significantly debated – however, it does appear that women who suffer pregnancy loss may have a larger number of these cells (but not all researchers agree).
Women with immune dysregulation may cause these cells to create a super inflammatory response, and (controversial) treatments to lower their numbers are currently being researched.
Antiphospholipid syndrome (APS) is an autoimmune disease with the presence of antiphospholipid autoantibodies formed against a person's own tissues. This interferes with coagulation and can result in miscarriage – as well as other pregnancy complications.
It is estimated that up to 42% of women suffering from recurrent loss may have APS. Treatment (low-dose aspirin and/or low molecular weight heparin) is not yet completely effective for all women with APS, and research remains ongoing.
A study published in May 2021 showed that the antiphospholipid antibody (aPL) positive rate was higher in females who failed in IVF/ICSI than those who succeeded in IVF/ICSI. This study also indicated that females positive for aPL have a higher miscarriage rate than those negative for aPL, but live birth rate, biochemical pregnancy rate and clinical pregnancy rate were similar between two groups.

Aspirin and heparin are widely used to reduce the risk of recurrent pregnancy loss in women with antiphospholipid syndrome. A case-based review published in March 2021 indicated that heparin (LMWH or UFH) plus aspirin may improve live birth rates in women with recurrent pregnancy loss and antiphospholipid antibodies, but evidence is of low certainty.
Untreated and undiagnosed Celiac Disease (CD), an inflammatory immune reaction to gluten, has been theorized to cause reproductive and pregnancy complications, such as infertility, miscarriage, and preterm delivery. Treatment with a gluten-free diet can prevent these negative outcomes. However, there is no evidence a gluten-free diet prevents miscarriage in women who have no immune response to gluten.
It’s been reported that undiagnosed CD may have such a causal effect on infertility and miscarriage that researchers advocate routine screening for CD in pregnant women – even in women without risk factors.
The argument is due to CD being considerably more common than most of the diseases for which pregnant women are already routinely screened (read more).
Obesity
It is currently assessed that some women who are considered obese may have an abnormal follicular environment, with smaller oocytes that are less likely to fertilize or implant normally. It has also been shown that women who are considered obese have a lower chance of pregnancy in any particular cycle than women who are not considered obese.
Further, although debated, higher rates of miscarriage have been associated with women who have a high BMI compared to women with a normal BMI, possibly due to inflammation. These results have led to the recommendation that women who are trying to conceive or have a history of miscarriage (especially recurrent) may have better success with weight loss (i.e. a reduction in their BMI).
It has been reported that even a moderate decrease of less than 10% in preconception weight improves maternal health and obstetrical outcomes.
Polycystic Ovarian Syndrome
Miscarriage and infertility are commonly associated with polycystic ovarian syndrome (PCOS), but not all studies agree. It is possible, however, that these positive associations are not due to PCOS itself, but other conditions related to the syndrome that cause fertility problems.
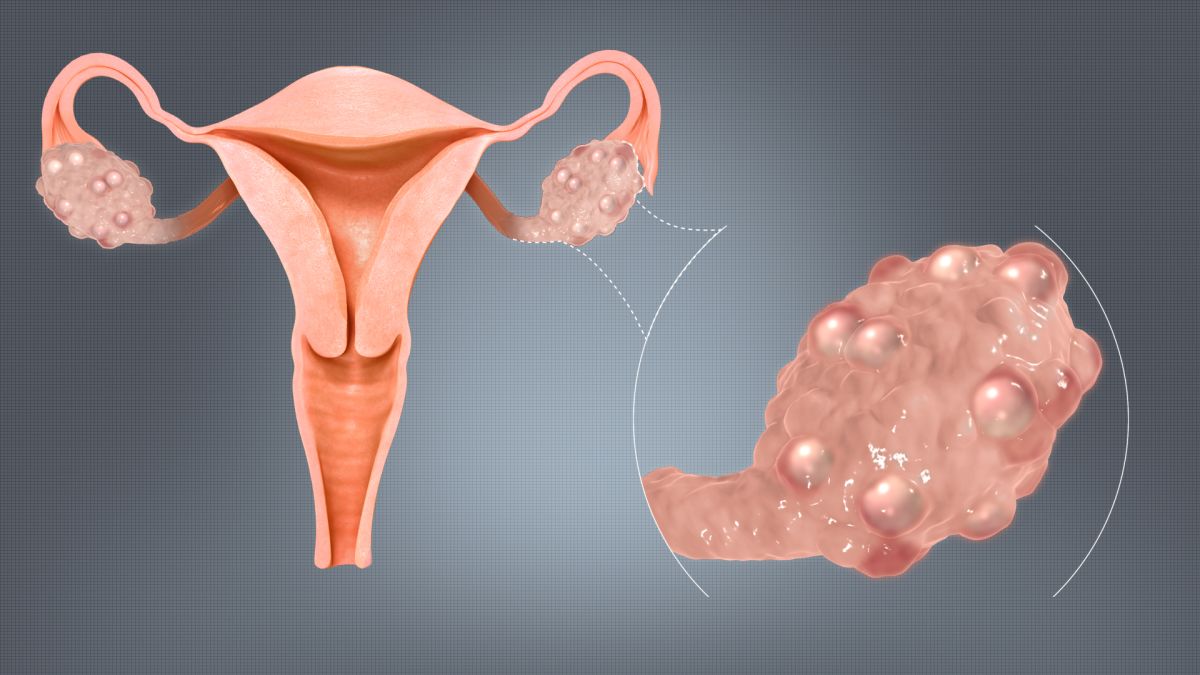
Insulin resistance and high BMI are the leading commonalities among women with PCOS that may be contributing to the higher rate of pregnancy loss.
Metformin is commonly used to treat insulin resistance but is also regularly stopped when pregnancy is confirmed. Research has been conducted to determine the safety and effectiveness of continuing metformin during pregnancy, specifically in the setting of PCOS.
However, results are inconsistent on its effectiveness and it is therefore not yet routinely recommended – but research remains ongoing.
Environmental
Environmental elements are considered “external” factors, such as malnutrition, medications, drugs, chemicals, and infections; these agents are also known as teratogens.
Until the 1950s, it was thought that embryos were protected from environmental elements and that medications (and other agents) did not pass through the placenta. Therefore, research into this aspect of pregnancy is considered new and vastly incomplete.
Researchers know a lot more about what environmental agents cause birth defects, as these are more easily tracked than miscarriage. Attempting to determine what type of chemicals, medications, or other exposures in the environment can cause miscarriage is very, very difficult, unless the association is somewhat obvious.
Miscarriage due to nutrition status is rare, and sole deficiency of one nutrient or moderate deficiencies in several does not appear to increase risks for miscarriage – even in extreme cases such as hyperemesis gravidarum.
However, nutrition during early development is associated with embryo/fetal growth, organ development, body composition and function. Further, adjustments in nutrient metabolism are apparent within the first weeks of pregnancy.
After fertilization, the fertilized egg and early blastocyst appear to detect and respond to the nutritional quality of the Fallopian tube environment, even before implantation.
Early nutrition status can also affect the development of the placenta, which in turn, is responsible for transporting nutrients and oxygen to the fetus.
Read more information regarding Nutrition.
Heat exposure, or anything that may elevate a woman's body temperature above 102 °F (to include a fever) is also considered a possible teratogen and potential cause of miscarriage.
Alcohol may also cause miscarriage, depending on timing, amount, and other factors.
Infection
Infections are not a very common cause of miscarriage, but certain infections at the time of conception may interfere with implantation.
Bacterial vaginosis is a strong risk factor for late miscarriage and is treated with oral clindamycin, an antibiotic. Women can learn more about the signs of vaginal infection here.
Chronic endometritis is defined as chronic inflammation of the endometrial lining, and some studies have shown an increased prevalence of this infection in women with pregnancy loss. The most widely used treatment appears to be an antibiotic regimen of doxycycline. This infection is not routinely checked by HCPs.
Sexually Transmitted Infections (STI) can also cause miscarriage as well as other pregnancy-related complications. STI testing during a preconception appointment is very important to ensure a healthy pregnancy right from the start. Further, women can contract an infection during pregnancy and completely miss the initial signs and symptoms. (read Herpes, Syphilis).
Helicobacter pylori (H. pylori) is a bacterium that causes gastrointestinal diseases. H. pylori is associated with miscarriage most likely as a result of its potential effect on placental tissue; the infection is treated with antibiotics.
Pregnancy itself may increase the susceptibility to H. pylori infection due to immune system changes. Interestingly, the infection is also linked to hyperemesis gravidarum.
The prevalence of H. pylori infection among pregnant women is estimated to be about 20% to 30% in most European countries, Japan and Australia, while it may be present in 50% to 70% of pregnant women in Mexico and Texas. It may also only cause problems in women more susceptible to it.

Influenza infection during pregnancy has been associated with miscarriage, as well as several other pregnancy-related complications. Influenza has been identified in fetal tissue, indicating the virus can pass through the placenta (but may be rare).
Although influenza infection has not be very well studied in early pregnancy, since early pregnancy requires an inflammatory response, it is possible contracting influenza at this time may create a “super inflammatory” response that can lead to miscarriage (read more).
There is no evidence influenza vaccination causes miscarriage (read more).
No "Morning Sickness"
In general, Nausea and Vomiting of Pregnancy ( NVP ) has been associated with a reduced risk of miscarriage. The mechanism by how this happens is not known. However, a lack of these symptoms is neither a cause of miscarriage nor does it present an increased risk of miscarriage.
Further, while NVP suddenly stopping during pregnancy has not been studied in regards to miscarriage, based on what is currently known about NVP, the absence or sudden absence of NVP does not indicate – by themselves – a pregnancy is in danger.
Physical Trauma
Physical trauma rarely causes first trimester miscarriage. However, major trauma – especially abdominal – can cause fetal loss as pregnancy progresses, especially in the third trimester.
Women who have been injured during pregnancy, or have taken a fall later in pregnancy, should always call their HCP or dial 911 in an emergency.
Action
For women who have experienced, or are currently experiencing a miscarriage, the feelings of guilt, frustration, confusion, and devastation can all be compounded by the inability to never know what caused it. Women should understand that current research indicates miscarriage is likely caused by more than one factor at the same time – most of which are beyond the control of both the woman and her partner.
Early assessment – and a preconception appointment – can potentially ease these emotions by possibly offering some type of assessment or management plan that can increase the chances of a successful pregnancy. Further, many women who experience even multiple miscarriages go on to have healthy, full-term pregnancies in the future.
According to The Lancet's Miscarriage Series published in April 2021, after one miscarriage, "women should have their health needs evaluated and be provided with information and guidance to support future pregnancies. If a second miscarriage occurs, women should be offered an appointment at a miscarriage clinic for a full blood count and thyroid function tests and have extra support and early scans for reassurance in any subsequent pregnancies. After three miscarriages additional tests, including genetic testing and a pelvic ultrasound, should be offered."
Women should not hesitate to ask their HCP about possible causes or screening tests. Although medicine does not have all the answers regarding human reproduction, in many cases, HCPs can provide women with more information and potential answers so women can make better informed decisions regarding their own reproductive health.
Resources
Early Pregnancy Loss (American College of Obstetricians and Gynecologists)
RESOLVE.org (Support Group)