Venous Thrombo-embolism

Venous thromboembolism (VTE) events, which include deep vein thrombosis (DVT) and pulmonary embolism (PE), are rare during pregnancy.
However, because swelling and shortness of breath are both common during pregnancy and are in some cases considered normal, VTE is therefore commonly suspected and considered, especially in the postpartum period.
The most common way to diagnosis DVT is through compression ultrasound, which is a safe procedure and can easily rule out DVT in one or two evaluations. Although PE diagnosis requires imaging/radiation, potential harm to the fetus is considered very, very low and the benefit of early diagnosis of PE can potentially safe a woman’s life.
If women experience sudden swelling in one leg along with redness, warmth, and pain in a specific spot on the leg – usually the left – this is more indicative of a possible DVT and women should call their HCP right away.
Women with DVT that leads to a PE can experience shortness of breath, swelling in one (sometimes both) legs, fatigue, and/or chest pain; this is considered an emergency and women should seek help immediately.
Again, VTE is rare during pregnancy, but if women or unsure or have any questions, they should call their HCP.
Background
There are various medical terms used to describe blood clots and different types:
Venous thrombosis: general term for when a blood clot occurs in a vein; veins are the blood vessels that take blood towards the heart and lungs; arteries take the blood away from the heart.
Venous thromboembolism (VTE): includes pulmonary thromboembolism and deep vein thrombosis; together, they occur in one in every 1,000 to 2,000 pregnancies, a risk that is 10 times higher than in non-pregnant women. The highest risk for all pregnant women is in the first six weeks after delivery.
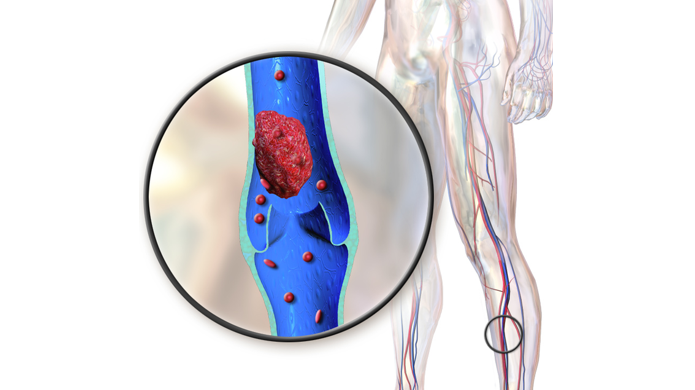
Deep vein thrombosis (DVT): a serious condition where a blood clot forms in a deep vein in the body, usually in the leg.
Pulmonary embolism (PE): a blood clot forms in the lower extremities that breaks off and travels to the lungs; considered an emergency; affects about 1 in 1000–3000 pregnant or postpartum women.
Although rare, VTE is considered one of the leading causes of maternal death during pregnancy and postpartum period. (Note: Actual clotting and bleeding times do not change.)
Fortunately, the vast majority of women who develop a clot will recover; mortality related to VTE is estimated at 1.1 to 1.5 deaths per 100,000 deliveries in North American and Europe.
Causes
Pregnancy predisposes women to VTE based on the physical changes that occur (and are necessary) to maintain a healthy pregnancy. The two most impactful changes include fluid buildup and slow blood flow. Compared to pre-pregnancy, blood has a much more difficult time leaving the lower body – especially in the third trimester.
The body retains an extra 6 to 8 liters worth of fluid during pregnancy which leads to swelling. Swelling is a potential contributing factor to the development of VTE, as well as a common first symptom of the condition. Swelling is also of the most common symptoms of pregnancy in general; therefore, this symptom can cause women significant anxiety.
Extra fluid is needed for amniotic fluid and blood volume expansion that aids in fetal growth and the prevention of blood loss during delivery. Blood volume, mostly plasma, increases gradually from 6 to 20 weeks of pregnancy and reaches a maximum volume around 32 to 34 weeks.

All this extra volume is slow to return to the heart from the lower body which causes fluid build up in the lower legs, feet, and ankles:
Early in pregnancy, blood pressure decreases; this, on top of the increase in blood volume, causes the lower veins to work harder (also causing varicose veins in the process). As pregnancy progresses, the growing weight of the uterus puts additional pressure on the inferior vena cava (vein from the pelvis to the heart), slowing fluid circulation even further.
Blood flow velocity in the lower limbs reduces by approximately 50% by the third trimester; standing in the same position or crossing the legs for an extended period of time increases the risk of blood building up in the veins, and can possibly lead to clotting.
A lack of physical activity can also cause swelling in pregnancy as exercise helps the body circulate blood and fluid out of the tissues and back into the lymphatic system.
Signs, Symptoms, and Complications
Although most pregnant women experience swelling during pregnancy, swelling related to VTE develops quickly (hours to days), and usually involves the left leg only – but not always. Women may also experience warmth, redness, and/or pain at the clot site, pain when flexing the foot, shortness of breath, and buttock, groin, or flank pain. Women should call their HCP immediately if they experience these signs/symptoms.
Although PE can occur from a deep vein in the leg, it has separate additional symptoms that include sudden difficulty breathing (shortness of breath), tightness or pain in the chest, coughing, coughing up blood, fatigue, and exhaustion due to a lack of oxygen. The risk of developing a PE is very small if DVT is diagnosed and treated.
It is important to note that DVT does not always have symptoms, so women should routinely stay hydrated, stay physically active, and talk to their HCP if they have any concerns.
Risk Level/Factors
There are many known potential risk factors, and therefore individualized risk assessments are recommended during pregnancy, which can also determine potential preventative methods.
The postpartum period poses the highest risk for VTE, including immediately after delivery and up to six weeks postpartum, after which risk significantly decreases.
Results of several studies show a higher rate of VTE in women who underwent cesarean delivery.

Varicose veins can be a risk factor, as the presence of varicose veins indicates the veins are already having a difficult time circulating blood. Read more.
Women with previous VTE have an approximately 3.5-fold increased risk of recurrent VTE in a subsequent pregnancy, compared to when they are not pregnant.
Additional risk factors include:
Having a condition that makes clots more likely (thrombophilia) **leading cause
Family history of blood clots
Over 35 years of age
BMI of 30 or more
Prior severe infection or trauma to a leg
Carrying multiple babies
History of fertility treatment
History of smoking (causes inflammation)
Labor lasted more than 24 hours
Significant blood loss after delivery
Receiving a blood transfusion
Several U.S. and international guidelines recommend women be assessed for VTE risk during preconception and again during pregnancy. HCPs need to discuss risks and benefits of women receiving long-term therapy with blood-thinning medications prior to conception.
Diagnosis
VTE diagnosis during pregnancy is difficult, but is also frequently considered given how common swelling and shortness of breath are as general symptoms of pregnancy. However, guidelines regarding the best way to diagnose VTE are not consistent, and most diagnostic and treatment studies of DVT have excluded pregnant women.
Compression ultrasonography (CUS) is now the imaging test of choice for diagnosing DVT. An HCP will examine the leg(s) and may recommend an ultrasound scan first to determine the possibility of thrombosis; repeat scans may be necessary.
Diagnosis of PE may include a chest X-ray and/or a CT scan; although both of these imaging scans use radiation, it poses little to no harm to the fetus; further, if PE is suspected, the benefits of the scan significantly outweigh any potential risk to the fetus.
Management
If VTE is diagnosed, the woman will may be advised to start treatment with an injection of an anticoagulant drug called heparin which thins the blood. The most used form in pregnancy is "low-molecular-weight heparin".
Heparin works to dissolve the current clot, prevents new ones from forming, and thereby reduces symptoms as well as the risk for PE.

Heparin is given as an injection under the skin at the same time(s) every day. The dose is determined by the woman's weight. Depending on when VTE is diagnosed, women are given the injections and taught how to use and dispose of them.
The medication causes bruising at the injection site that fades in a few days. Approximately 1 to 2 in every 100 women will have an allergic reaction. Women should immediately notify their HCP if they notice a rash developing after an injection.
Heparin is safe during pregnancy: the drug does not cross the placenta, does not affect the baby, and does not enter breast milk.
Recommendations regarding the drug’s use near and at delivery vary; there are no large trials of anticoagulants in pregnancy and recommendations are based mostly on published case studies and clinical experience.
All pregnant women receiving anticoagulants should have an individualized delivery plan that addresses all health concerns, as well as the risk of taking the drug versus possible heavy bleeding the drug may cause at delivery.
However, in general:
Women are usually advised to stop injections if they think they are in labor. Women who are scheduled to be induced or deliver via cesarean section usually stop the medication 12 to 24 hours prior to induction; the medication will likely be restarted within 12 to 24 hours after delivery.
Induction of labor may be recommended as this helps prevent the risk of labor occurring on full anticoagulation, likely reducing the risk of bleeding and giving the woman all options for pain relief.
If a woman needs to delivery immediately via cesarean section and she was on full heparin, she cannot receive a spinal or epidural, and will require general anesthesia.
Continued treatment with heparin (injections/tablets) is recommended until at least six weeks after delivery, with a minimum treatment time usually three months in total.
Regarding preventative (prophylactic) use of heparin during a subsequent pregnancy, or in women assessed to be at high risk for VTE, the evidence is very uncertain about benefits and harms of this prevention method in women during pregnancy and the early postnatal period. This decision needs to be made between a woman and her HCP, and needs to involve all possible known risks and benefits of using the medication.
Action
Women should call their HCP immediately if they experience any of the signs/symptoms described above.
Compression therapy is commonly recommended for swelling, varicose veins, and the prevention of VTE as it can help circulation in the legs. Compression does appear to reduce the severity of current DVT as well as symptoms (30 to 40 mm Hg strength).
There are many "modern" versions of these garments currently available online that make them appear as regular, "higher fashion" socks (vs. the "nylon" style of years past).
Exercise and frequent movement is also recommended as exercise can help circulate the blood/fluid in the legs.

It is important to note that DVT does not always have symptoms, so women should routinely stay hydrated, stay physically active, and talk to their HCP if they have any concerns.
Women should consider sharing their experience (below) regarding suspected or diagnosed VTE during pregnancy. The possibility of a blood clot can make women very anxious and nervous, especially in the setting of swelling. Any exposure to women's experiences with the condition can help women learn more about these events and when to call an HCP.
Partners/Support
Partners, family members, and other support members of pregnant women can play a role in assisting wonen's reduction of risk, as well as any potential delay in diagnosis of VTE during the woman's pregnancy.
Support can encourage women to stay active, avoid standing/sitting for long periods, and to rest and put their feet up occasionally throughout the day – especially in the third trimester.
Further, although rare, support members should learn the signs and symptoms of VTE described above, especially in the case of PE. Signs/symptoms may come on quickly, and if women are experiencing shortness of breath and extreme fatigue, they may not be able to fully communicate (including the postpartum period). It is possible that support members may notice these signs first, before the woman herself.
Resources
What is Venous Thromboembolism? (U.S. Centers for Disease Control and Prevention)
Preventing Deep Vein Thrombosis (American College of Obstetricians and Gynecologists)
Reducing the Risk of Venous Thromboembolism during Pregnancy and the Puerperium (Royal College of Obstetricians and Gynaecologists)
Air Travel and Pregnancy (Scientific Impact Paper No. 1) (Royal College of Obstetricians and Gynaecologists)