Cardiovascular System

Unlike all other organ systems in the embryo, the cardiovascular system needs to function almost as soon as it starts to form.
The heart starts beating at the beginning of five weeks of pregnancy, while the rest of the heart continues to develop with blood already running through it.
Once the embryo can be observed via ultrasound with a heart rate comparable to its gestational age, the rate of miscarriage drops significantly, even well before 12 weeks of pregnancy.
Further, due to advances in technology, it is rapidly becoming more feasible to better evaluate all structures of the heart in the first trimester – despite the heart being only a few millimeters in size.
Pregnant women with questions related to their baby's heart development, heart rate, or viability in the first trimester, should read more information below and talk to their HCP.
Background
The cardiovascular system is the first organ system to be functional in the embryo, and includes the heart, blood, and blood vessels (arteries, veins, capillaries).
Heart development is a complex process involving over 500 genes in which the heart transforms from a single tube to a fully septate heart with four chambers.
Early Pregnancy
The fetal heart needs to function almost as soon as it starts to form.
Gastrulation is the process in which the three foundational layers of the early embryo are developed: ectoderm, mesoderm, and endoderm. All tissues and organs are developed from these three layers.
The heart forms from the mesoderm layer around 18 to 19 days after fertilization, or between 4 and 5 weeks of pregnancy, with the formation of the primitive heart tube. Five "dilations" appear along the tube that eventually form all adult structures of the heart.
The heart begins beating at the very beginning of week 5, or 21 to 23 days after conception and then begins to loop. A network of blood vessels begins about 7 days later which can be detected by Doppler ultrasonography. Most of the heart’s structure is formed while the heart is already pumping blood.
This image contains triggers for: Real Embryo
You control trigger warnings in your account settings.
The presence of fetal heart activity after 5 to 6 weeks of pregnancy, or once the embryo reaches 2 millimeters (mm) in length, is associated with a less than 3% to 6% risk of pregnancy loss. This risk decreases even further if this is seen after 8 weeks.
Since the heart starts beating by 5 weeks and becomes partitioned into four chambers by 9 weeks, the critical period of development for the heart is considered to be 5 to 9 weeks of pregnancy. During this time, the heart begins as thin walled tubes which then fuse, the heart contracts, the tube lengthens, and septation starts. Any deviation from this pattern at any time could result in one or more congenital heart defects.
At the end of 9 weeks of pregnancy, the heart has developed to its mature form and may measure 3 to 4 mm near 10 weeks (vs. 1 to 1.5 mm at 6 weeks).
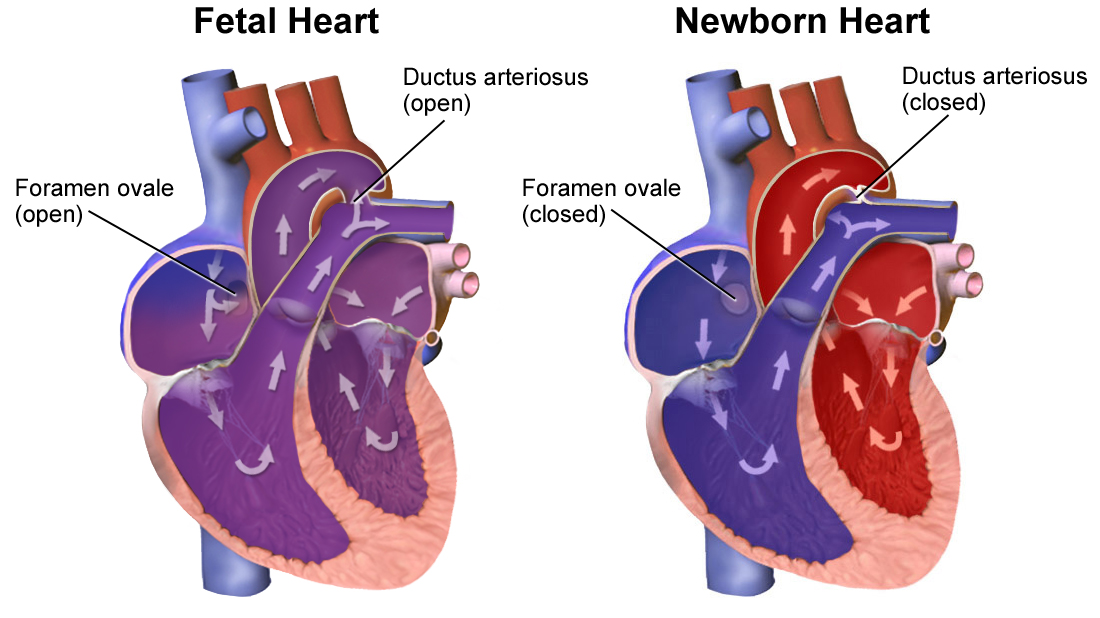
In the fetal heart, there are two structures that allow blood to bypass the lungs, since the lungs are filled with fluid during development, not air.
The ductus arteriosus is a short, open blood vessel that connects the pulmonary (lungs) artery to the aorta. This blood vessel is open so that oxygenated blood can bypass the pulmonary circulation (see diagram below). The ductus arteriosus closes within a few hours to days after delivery as the baby breathes in oxygen for the first time (failure of this to close is called Patent Ductus Arteriosus).
The foramen ovale is an opening (or shunt) in the heart that allows blood to flow from the right atrium to the left atrium, also bypassing the pulmonary circulation. After delivery and when the fetus attempts to breathe, this pressure forces the opening to close over time, usually between 6 to 12 months of age. Failure of the foramen ovale to close is called Patent Foramen Ovale, or a "hole in the heart".
Heart Rate
In healthy fetuses, the heart rate increases from approximately 110 beats per minute (bpm) at the 5th week of pregnancy to 170 bpm by the 9th week. From then on, there is a gradual reduction in the heart rate to about 150 beats per minute by the 13th week. This decline is thought to be the result of a well-developed parasympathetic nervous system, which slows the heart rate.
Pregnancies in which the embryo has a rapid early heart rate have a good prognosis, with a high likelihood of normal outcome; however, the boundary between slow and normal heart rates has not been definitively established.
Slower heart rates can also be normal; it is possible that 100 bpm up to 6 weeks 2 days of pregnancy and 120 bpm at 7 weeks of pregnancy can occur in normal pregnancies, and is likely considered the lower rate of normal.
Research has also indicated that fetal heart rates below 90 bpm at 6 weeks, or below 110 bpm at 8 weeks of pregnancy have been shown to be associated with a very high risk of miscarriage (as long as gestational age is correct).
Congential Heart Defects
With rapid improvements in medical imaging, it is becoming possible to diagnosis congenital heart defects in the first trimester. A review published in August 2021 indicated that examination of the heart in the first trimester allows identification of over half of fetuses who are highly likely to be affected by major heart defect.

Cardiac congenital defects represent about 20% of all birth defects, or 5 to 8 of every 1,000 live births – the causes of which are mostly unknown. While some heart defects are linked to genetics, others are linked to certain environmental factors such as alcohol, lithium (as a medication), and retinoic acid, as well as diabetes and rubella.
The current leading theory assesses heart defects are caused by numerous variables, mostly outside factors that serve as “triggers” to a genetic make-up that is susceptible to disturbances from these factors. Meaning, certain individuals have a genetic make-up that makes them more vulnerable to certain elements in the environment that may trigger the development of birth defects.
Action
Pregnant women with questions related to their baby's heart development, heart rate, or viability in the first trimester should talk to their HCP, as well as a genetic counselor, if recommended.
Resources
Fetal Circulation (American Heart Association)
Heart Development (UNSW Australia; Dr. Mark Hill)