Blood Volume

Blood volume increase is one of the most significant changes to the body during pregnancy, after the enlarging uterus.
Blood volume increases almost 50% during pregnancy, starting in the first trimester. Proper blood volume increase ensures healthy fetal and placental growth and development as well as adequate protection against blood loss during delivery.
However, this increase can cause a significant number of potential symptoms, conditions, body changes, and nutrient deficiencies all of which are considered normal occurrences during pregnancy (i.e. fatigue, dehydration, swelling, anemia, urinary frequency).
Learning about blood, blood volume, and its associated changes during pregnancy can help women better understand what their body is doing and why they are feeling so many different symptoms early in pregnancy.
Background
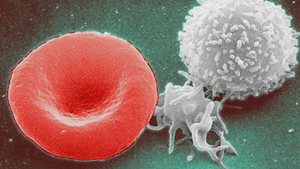
Blood has four components: plasma, red blood cells, white blood cells, and platelets; these are essentially “mixed together” as the blood in veins and arteries.
Blood volume refers to the total amount of fluid circulating within the arteries, capillaries, veins, and chambers of the heart at any time.
An average sized non-pregnant woman has about 9 pints of blood (4.25 liters).
Pregnancy
Total blood volume during pregnancy increases by about 1.5 liters (almost 40% to 50% increase, or about 1,250 to 1,500 milliliters) to support fetal and placental development and protection from blood loss during delivery. Around 1 liter of blood alone is contained within the uterus and maternal blood spaces of the placenta.
Blood volume (mostly plasma) increases gradually from 6 to 20 weeks of pregnancy and reaches a maximum volume around 32 to 34 weeks.
Even by 12 weeks, plasma volume (the "clear" part of the blood) expands by approximately 15% compared with prior to pregnancy. Further, this increase appears to directly and positively correlate (i.e. good sign) with fetal and placental weight. A bigger baby, or carrying two or more babies, further increases blood volume.
Blood volume increase during pregnancy is necessary, but it can also cause symptoms such as swelling, fatigue, anemia, deep vein thrombosis, dehydration, and urinary frequency (due to the increase in plasma).
A lack of blood volume increase has been implicated in outcomes such as preeclampsia, fetal growth restriction, and preterm birth.
Pregnant women are advised to stay hydrated in order to support the growing amount of both amniotic fluid and blood volume. Hydration may also help alleviate fatigue, which also begins (and peaks) in the first trimester.

Interestingly, the presence of an embryo is not needed for a blood volume increase, as significant changes have also been seen in women with a molar pregnancy.
Red Blood Cells
Red blood cells give blood its red color, and make up about 40% to 45% of total blood volume. These cells are made in the bone marrow and then transported to the bloodstream.
Red blood cells increase by about 250 ml (18%) during pregnancy (compared to 40% to 50% for plasma).
In order to make these additional red blood cells that are necessary during pregnancy, a pregnant woman requires more iron.
Pregnancy causes a two- to three-fold increase in the requirement for iron, a 10- to 20-fold increase in folate, and a two-fold increase in the requirement for vitamin B12 in order to make hemoglobin (the iron containing part of red blood cells) and carry out other functions.
Women who take iron, B12, and/or folic acid supplements may have a greater increase in red cell mass, up to an additional 200 to 250 ml.
Plasma
Blood is comprised of about 55% plasma – a mixture of water, sugar, fat, protein, and salts. Plasma is needed in much larger amounts than red cell mass due to the extra blood flow to organs. This dramatic increase in plasma is also the primary cause of swelling during pregnancy.
Because there is a greater increase in plasma than red cells, red cells in the blood are "diluted". Therefore, even though the body has made more red blood cells than it had prior to pregnancy, blood tests usually indicate mild anemia, which is considered normal during pregnancy.
However, this could also potentially “hide” real deficiencies in folate, iron, or vitamin B12; HCPs may routinely check plasma levels of these vitamins in the mother’s blood (anemia can be caused by a lack of folate and B12 as well, not just iron).
The lowest drop in hemoglobin is usually around 34 weeks of pregnancy.
Normal hemoglobin values are cited as 10 to 13 g/dl. The majority of women who have a hemoglobin level lower than this will be considered to have pregnancy-induced anemia and are recommended to receive iron supplementation. Folate and B12 may also be given, and in some instances, can be given instead of iron.
White Blood Cells
White blood cells, which fight infection, account for about 1% of total blood volume. These cells are also increased during pregnancy due to the physiologic stress induced by pregnancy, mostly in the third trimester.
Interestingly – labor, and the first few days after delivery – bring about a marked increase in white blood cells. Although this is not clearly understood, it is hypothesized to be the stress of delivery. Levels return to non-pregnant levels around four weeks postpartum.
A significant, acute (sudden) rise in white blood cell count outside of labor could be caused by an infection and will likely require further testing.
Platelets
Platelets are small fragments of cells that help blood to clot at the site of an injury.
Large studies have determined that platelet count tends to fall gradually during pregnancy, especially in the third trimester. This fall is likely due to the increased use of white blood cells from the mother within the uterine and placental circulation.
However, despite this fall in platelets, pregnant women are still at higher risk for venous thrombosis events due to the slow return of blood from the legs, which allows it to pool and clot; the growing uterus also puts pressure on veins, further slowing blood flow.
Therefore, normal pregnancy is characterized by an increase in platelet collection at various locations throughout the body, but a decrease in total number.
Delivery and Postpartum
Typical loss of blood during/after delivery equals approximately 300 to 500 ml for vaginal births, and 750 to 1,000 ml for cesarean sections.

To protect against this loss, blood volume increases during labor, as uterine contractions squeeze blood out of the intervillous spaces of the placenta and into the mother’s circulation.
The same thing occurs right before placental removal, as an infusion of additional blood occurs as the uterus contracts after delivery.
Blood volume slowly returns to normal about eight weeks postpartum, which mainly occurs as the extra plasma is excreted through frequent urination.
Action
For women who experience significant fatigue early in pregnancy, they should ask their HCPs about about their iron, folate, and/or B12 levels. Note: Women should never take supplements during pregnancy without speaking to their HCP first.
It is recommended that pregnant women exercise and stay hydrated to help their bodies adjust to the increase in blood volume and to prevent its associated symptoms. However, it is unclear how much pregnant women should drink in comparison to non-pregnant women (read Hydration and Thirst).
Resources
Introduction to Blood and Blood Volume (BC Open Textbooks)