Eyes and Vision

Pregnancy can increase the risk of numerous eye and vision changes – most of which reverse postpartum. These changes can lead to symptoms that may be very unexpected for some women, but fortunately are considered mostly harmless.
These changes (red eye, blurry vision, dry eye, pigmentation, contact lens discomfort) occur due to the significant blood and fluid volume increase that begins very early in pregnancy, as well as the increase in various reproductive hormones that have receptors in the eye.
Although these changes are common, and in most cases are due to pregnancy, women should always tell their HCP about any eye-related changes they experience. Certain eye changes can be “red flag” symptoms for high blood pressure, preeclampsia, and eclampsia, and are critical for pregnant women to recognize – especially those at risk.
Further, some eye changes may be unrelated to pregnancy and therefore require evaluation by an HCP. It is also recommended that women with certain medical conditions, such as diabetes or Graves’ disease, receive an eye exam prior to pregnancy, as well as during the first trimester.
Background
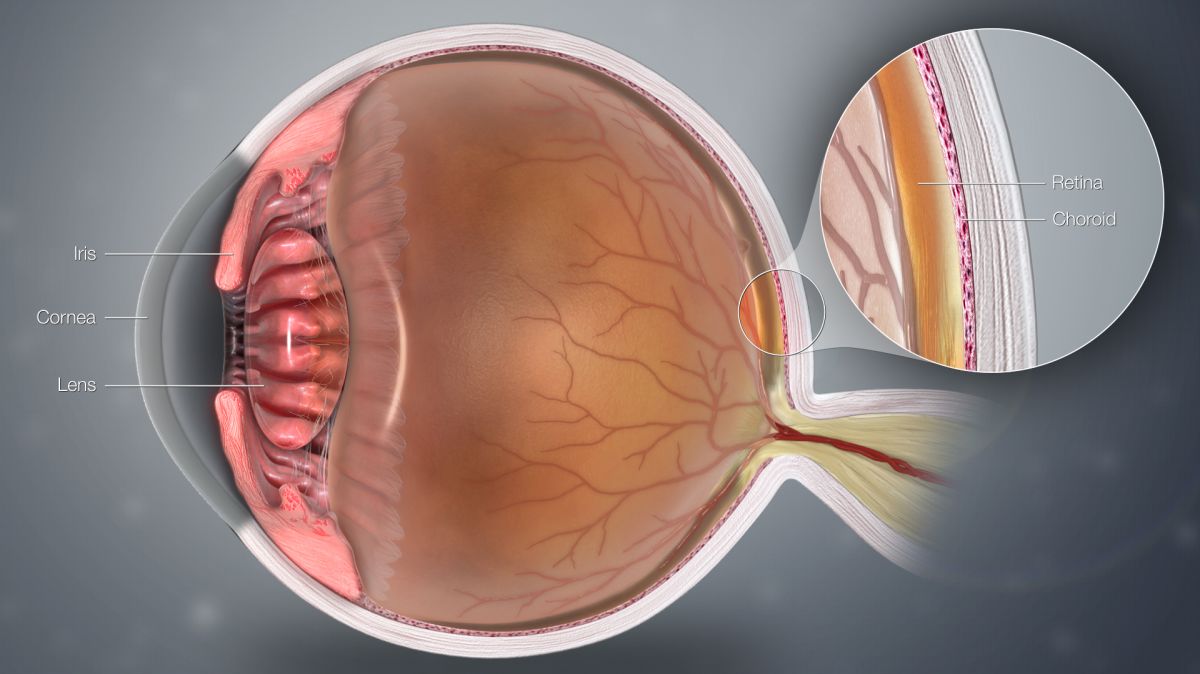
Pregnancy-related changes in the eye can affect the eyelid, conjunctiva (mucus membranes), cornea, lens, retina, optic nerve/tract, and orbit. As a result, symptoms may include vision changes, dry and/or red eyes, contact lens discomfort, eyelid drooping, and various pigment changes in and around the eye.
Most eye/vision changes during pregnancy occur due to hormones. Receptors for female reproductive hormones (progesterone, estrogen) are present in all components of the eye. When pregnancy causes an increase in these hormones, the entire eye is affected, but some women notice these changes more than others.
This is in line with symptom severity, which appears to be strongest in the third trimester, when hormone fluctuations are at their peak. Fortunately, since hormones affect/cause these changes, almost all symptoms go away shortly after delivery and are rarely permanent.
General Changes and Symptoms
Skin pigmentation, which is common in general during pregnancy, can extend from the cheeks to around the eyes and on the eyelids, which usually fades postpartum.
Ptosis (drooping of the eyelids) has been reported during pregnancy, to include during labor and delivery and in the postpartum period; it is thought to be related to fluid retention, stress, and hormonal changes. It is often in one eye only, requires no treatment, and usually resolves postpartum.
Dry eye is also common because reproductive hormones decrease natural tear production. If dry eye is left untreated, it can be harmful and could lead to tissue damage and scarring that can impair vision. Dehydration can worsen dry eye. Lubricating eye drops can help and are safe to use during pregnancy, after discussion with an HCP; dry eye usually resolves postpartum.
A September 2020 study of 106 pregnant women found a statistically significant increase in tear production in the immediate postpartum period.
Pregnancy causes improvement in autoimmune diseases such as non-infectious uveitis, which is inflammation of the middle layer of the eye. In women who are diagnosed with uveitis, the disease appears to be relatively inactive during pregnancy, but rebounds within six months of delivery. Uveitis is treated by using eye drops or other medications.
Although conclusions are slightly inconsistent, it is believed decreased ocular pressure also occurs during pregnancy (measurement of fluid pressure in the eye) but is considered normal. Small amounts of fluid regularly move in and out of the eye in equal amounts; when this is unequal, a decrease or increase in pressure results.
These changes typically return to pre-pregnancy levels by two months postpartum. This decrease does not usually result in symptoms but could cause blurry vision.
Glaucoma improves during pregnancy due to this decrease in pressure and few cases of glaucoma are diagnosed during pregnancy.
A Krukenberg spindle (pigment on the cornea) occurs in about 3% of pregnant women. Krukenberg’s spindle may appear in the first two trimesters; in the last trimester and postpartum, the spindle shrinks and disappears. A photograph of this condition can be viewed here.
Conjunctival hemorrhage (hyposphagma – ruptured blood vessel) is harmless and can be seen in about 10% of women during and after delivery, or in women with severe vomiting due to hyperemesis gravidarum. It requires no treatment, but blood pressure may be monitored by an HCP.
Vision Changes
Impaired vision is a common complaint during pregnancy either alone or in association with other complications and symptoms. Fluid retention causes changes in eye structure and shape which can result in refractive changes. Refractive errors can cause nearsightedness, farsightedness, and loss of near vision.
A temporary lessened ability to focus the eye (which usually happens with aging) is possible with pregnancy and lactation.
Night blindness can occur during pregnancy (mostly in developing countries) caused by vitamin A deficiency, which is treated with supplementation.
Bitemporal loss (type of partial blindness), concentric constriction, and enlarged blind spots can be experienced during pregnancy and are completely reversible after delivery. MRI studies have shown that the size of the pituitary gland increases during normal pregnancy and could press on or damage the optic chiasm (where the optic nerves from both eyes cross) causing partial blindness.
Corneal lens thickness increases during pregnancy, and with lessened tear fluid as mentioned above, can cause potential and temporary nearsightedness in about 10% to 15% of pregnant women.
Contact Lenses
Most studies – but not all – have determined that corneal thickness and curvature increases, while its sensitivity decreases due to hormones and fluid retention, which leads to “contact lens intolerance”.
This intolerance resolves completely after delivery or after breastfeeding is stopped, but contact lens use that becomes painful may traumatize the cornea and should be discontinued until these changes subside.
Since these issues resolve postpartum, it is advisable to delay fitting and prescribing new glasses or contact lenses until several weeks to six months postpartum. Most of these refractive changes are temporary, but a small number of women may experience a permanent change to their prescription.
Note: A woman can have contact lens issues during one pregnancy but not during another.
Refractive surgery, such as LASIK®, is very unpredictable during pregnancy due to the above described changes. It is recommended that refractive procedures in pregnant women be postponed until after delivery, since most changes are only temporary.
A February 2021 case series review (Spain) of pregnant women who underwent LASIK or surface ablation found increased efficacy, predictability, and safety risks associated with the procedures vs. women who were not pregnant. No complications of pregnancy or labor were reported. The authors indicated they "do not recommend performing LASIK or Surface Ablation on pregnant women."
Preeclampsia (and Hypertensive Retinopathy)
Any type of vision change is always a concern during pregnancy in the event it is related to a hypertensive disorder. It is estimated that 25% to 100% of pregnant women with severe preeclampsia and 50% of women with eclampsia experienced at least one vision change.
First documented in 1855, most of the visual disturbances during pregnancy that are the result of hypertension or preeclampsia tend to reverse in the postpartum period. However, women still require immediate medical attention for early, necessary management of these conditions.
Blurred vision is the most common symptom of preeclampsia, (but does not always mean a woman has preeclampsia) and requires a call to an HCP. Preeclampsia is also associated with color vision changes, a decreased visual field, obstructed vision, blind spots, double vision, and complete loss of vision or retinal detachment. Symptom severity generally matches the severity of hypertension and/or preeclampsia/eclampsia.
It is theorized these symptoms may be caused by extra fluid, retinal vasospasm, and resistance to blood flow due to the narrowing of blood vessels due to high blood pressure.
Cortical blindness, which affects up to 15% of preeclamptic and eclamptic women, is often preceded or accompanied by headache, eye twitching, and eye muscle weakness.
Retinal detachment, the most serious vision-related consequence of hypertension may occur in approximately 1 in 18,524 pregnancies, or 1% of preeclamptic women, and 10% of eclamptic women. Exudative retinal detachment tends to affect both eyes, is usually diagnosed postpartum, and may be more common in women who had a cesarean section.
Preeclamptic and eclamptic women with HELLP syndrome may be approximately seven times more likely to develop a retinal detachment.
Fortunately, it tends to resolve completely postpartum. Symptoms include various vision-related changes to include blurred vision, floaters, black spots, shadow-like curtain, and flashes of light.
Graves' Disease
Women diagnosed with Graves' disease (overactive thyroid) will commonly experience eye-related symptoms during pregnancy. Graves' disease tends to worsen in the first trimester, lessen in the second and third trimesters, and worsen again postpartum. Depending on severity, anti-thyroid medication may or may not be required.
Women who were diagnosed with diabetes or Graves' disease prior to pregnancy may experience the most significant and potentially serious and permanent eye changes. The American Academy of Ophthalmology recommends that women with predisposing conditions such as diabetes or Grave’s disease who plan to become pregnant should ideally have a dilated eye exam before pregnancy.
Diabetic Retinopathy
The number of women with diabetes in pregnancy is increasing, and therefore pregnancy is becoming associated with an increased risk of development and progression of diabetic retinopathy. Diabetic retinopathy occurs when high blood sugar levels cause damage to blood vessels in the retina.
During pregnancy, diabetic retinopathy can progress quickly, and its severity depends on the woman’s medical history, the degree of the disease prior to pregnancy, how well it’s been managed, and any other co-existing medical conditions.
Women with diabetes should have an eye exam prior to pregnancy, and an exam during the first trimester. The disease can progress even up to one year after delivery, so eye exams/monitoring should continue regularly.
If a woman is diagnosed with gestational diabetes but did not have pre-existing diabetes, this does not seem to increase the risk for diabetic retinopathy.
Action
Women need to tell their HCP if they experience any change to their eyes/vision; some HCPs will want to see women experiencing vision-related symptoms the same day. Women may also be referred to an ophthalmologist (a physician specializing in eye and vision health).
Resources
Parts of the Eye (American Academy of Ophthalmology)