Abdominal Pain

Abdominal pain during pregnancy is common; however, the determination of the cause of the pain is complicated and can be frustrating for both women and their health care providers (HCPs).
Abdominal pain during pregnancy can be related to pregnancy itself, or can be triggered by non-obstetric causes that happen to occur during pregnancy.
Pregnancy causes many aspects of the abdomen to change, including the location of certain organs; normal techniques an HCP would use to assess abdominal pain are not applicable during pregnancy.
Therefore, investigation during pregnancy requires imaging (ultrasound, MRI, and/or CT scans) and numerous laboratory-related screenings (blood, urine).
Women should always bring abdominal pain (and bleeding) to the attention of their HCP or, if severe, to the emergency department. Certain conditions such ectopic pregnancy and appendicitis are considered emergencies and need to be ruled out.
Background
Abdominal pain throughout pregnancy is common and is usually related to the pregnancy itself. However, abdominal emergencies during pregnancy that are not related to pregnancy occur in 1 of 500 to 700 pregnancies, with appendicitis and gallstones being the most common.
Diagnosing and evaluating pregnant women with abdominal pain is complicated. Common symptoms of pregnancy such as nausea and vomiting, cramps, round ligament pain, heartburn/reflex, gallstones, and uterine stretch can mask other causes of abdominal pain and delay diagnosis of potential emergencies (i.e. appendicitis).
Possible pregnancy-related causes of abdominal pain include:
Ectopic pregnancy (pain occurs around 6 to 14 weeks of pregnancy and needs immediate evaluation)
Preeclampsia or HELLP syndrome (right upper quadrant pain)
Chorioamnionitis (infection of fetal membranes)
Placental abruption (also usually includes bleeding)
Placenta Previa (usually painless, but can present with pain)
Uterine rupture (bleeding also present)
Acute fatty liver of pregnancy
Acute polyhydramnios (excess of amniotic fluid)
Uterine torsion
Labor pain (including preterm)
Non-pregnancy-related causes of abdominal pain that can occur during pregnancy include:
Appendicitis (most common)
Cholecystitis and gallstones (most common)
Gastroenteritis (“stomach bug”)
Fibroid(s)
Torsion of the ovary or fallopian tube
Ovarian cyst(s) (usually resolve on their own during pregnancy)
Intestinal obstruction
Peritonitis
Abdominal trauma
Meckel’s diverticulitis
Peptic ulcer
Acute pancreatitis (rare, usually the result of gallstones)
Diagnosis
The evaluation of abdominal pain in a pregnant woman is very challenging for an HCP. Pregnant women can be affected by the same causes of abdominal pain as the general population, as well as many others that are related to pregnancy.
Further, the anatomical changes of pregnancy displace organs from their normal positions; therefore, the palpation or “feeling” of the abdomen that HCPs normally perform to assess abdominal pain is not as effective during pregnancy.
Assessment of abdominal pain during pregnancy can also be inaccurate, leading to a delay in diagnosis that can be dangerous. When this occurs, it could lead to possible exploratory laparotomy (surgery to determine cause), increased imaging studies, premature delivery, and/or cesarean section.

Ultrasound is safe during pregnancy and is the top recommended initial diagnostic test. MRI (no radiation) is the next recommended imaging step if ultrasound is inconclusive, especially for appendicitis. A CT scan (radiation) may also be required if a potential emergency is suspected.
If a CT is recommended during pregnancy, it is likely the benefit of the resulting image outweighs the risk of the radiation (which is very, very small) and steps can be taken to minimize any potential exposure.
Diagnosis tests may include urine dipstick, glucose monitoring, fetal monitoring, blood tests, electrocardiogram (EKG), ultrasound, chest X-ray, MRI, CT scan, and possible pelvic examination as long as infection and/or placental concerns are not suspected.
Appendicitis
Appendicitis is the most common cause of non-obstetric pain in pregnant women, and appendectomy is therefore the most common non-obstetric surgery performed, occurring in approximately 1 in 1,000 to 1,500 pregnancies.

The outcome of pregnancy in a woman diagnosed with appendicitis is dependent on the timing of the diagnosis, similar to the general population. Early, uncomplicated appendicitis is estimated to result in potential fetal death in 4% of cases (the woman in up to 5%), but this increases to 20% to 30% for the fetus if the appendix ruptures. This significant increase is attributed to the delay in diagnosis that usually occurs in pregnant women.
Women should bring all abdominal pain they are experiencing to the attention of their HCP or emergency room if severe.
Symptoms of appendicitis during pregnancy are similar to those who are not pregnant; however, the location of the abdominal tenderness may be different depending on the size of the uterus and can be much higher than otherwise expected. An enlarged uterus may shift the appendix from the right lower quadrant to the right upper quadrant, which also causes confusion for HCPs.
Pain may initially present as quite severe, near the belly button, and expanding to the right lower or right upper quadrant of the abdomen. Symptoms may also include nausea, vomiting, fever, bloating, constipation or diarrhea, and pain with movement.
Treatment: Appendicitis is a medical emergency and the appendix must be removed surgically. The risk of surgery is considered insignificant compared with the risk of waiting and allowing rupture to occur. Laparoscopic appendectomy is safe and effective during pregnancy and usually poses no additional risks to a pregnant woman than a non-pregnant woman.
Gallstones
This section overlaps with Gallbladder, Liver, and Pancreas Body Changes during pregnancy.
Gallbladder motility, essentially the speed at which it can release bile (a digestive fluid) into the small intestine, slows down during pregnancy due to progesterone. This is assessed to play a large role in gallstone formation.
Progesterone has an inhibitory effect on the ability of smooth muscle to contract, such as the stomach, uterus, and the gallbladder.
For example, high levels of progesterone during pregnancy stop the uterus from contracting, until term, in which progesterone levels drop so the uterus can contract. This process is similar for the contractility of the gallbladder, which therefore also slows down. This can cause gallstones or sludge to form in some women.
Gallstones are hardened deposits of bile that form within the gallbladder. A stone can be as small as a grain of sand or as large as a golf ball.

Gallbladder disease (gallstones/sludge) is already four times more common in women than men, and pregnancy increases this risk even further. Gallbladder sludge or gallstones develop in approximately 31% and 5% of pregnant women respectively, and is a common cause of hospitalization, even up to one year postpartum.
Gall sludge or stones that do not cause symptoms do not need treatment, as this condition generally resolves after delivery. However, some women may have symptoms that increase afterward, and removal of the gall bladder can be necessary in the postpartum period.
Pregnant women who develop gallstones are closely monitored. If a gallstone blocks the gallbladder or causes an infection, surgery may be necessary.
Gallbladder surgery (cholecystectomy) is the second most common non-obstetric-related procedure during pregnancy and numerous studies indicate this surgery is safe for pregnant women and the fetus. While the surgery can be performed in any trimester (but is best in the second trimester), risks and benefits may need to be discussed with a health care provider.
Bowel Obstruction
In some cases, severe constipation can lead to possible bowel obstruction, which is estimated to be the third most common gastrointestinal emergency that can arise during pregnancy with an incidence of 1 in 2,500 deliveries (behind appendicitis and gallstones).
Pregnant patients commonly present with bowel obstruction in the third trimester likely due to the uterus causing additional digestive issues on top of hormonal effects.
Diagnosing bowel obstruction in a pregnant woman is difficult due to pregnancy itself. Further, the presenting symptoms of obstruction include nausea, vomiting, and abdominal pain, which are symptoms commonly present in pregnant women for numerous other reasons.
Ultrasound and MRI are the most commonly used imaging techniques in pregnant women to diagnosis bowel obstruction since neither include radiation risk.
The treatment of intestinal obstruction in pregnant women is similar to non-pregnant women and usually requires hospitalization. Delivery via cesarean section may be required depending on gestational age and severity of the obstruction.
The use of intravenous fluids and a nasogastric tube together with the avoidance of food and close monitoring can help maintain hydration, relieve pressure, and allow the obstruction to possibly pass on its own. Surgery may be needed in cases of complete blockage. The risks of not having surgery could be fatal to both mother and baby and would outweigh any potential risks of the surgery itself.
Pancreatitis
Although pancreatitis is a rare cause of abdominal pain during pregnancy, occurring in 0.1% to 1% of pregnancies (most commonly in the third trimester), it can be a complication of gallstones, which is very common during pregnancy.
Acute pancreatitis is the sudden inflammation of the pancreas resulting in pain, nausea, and vomiting that requires immediate treatment to avoid life-threatening complications. The inflammation occurs as the pancreas’ digestive enzymes start digesting the pancreas itself.
There are many causes of acute pancreatitis – the two most common are alcohol use and gallbladder/bile duct disease, the latter being the most common cause during pregnancy. It is thought that with the hormonal changes induced by pregnancy, gallstones are more likely to form and thus travel down the common bile duct to obstruct the pancreatic outflow.
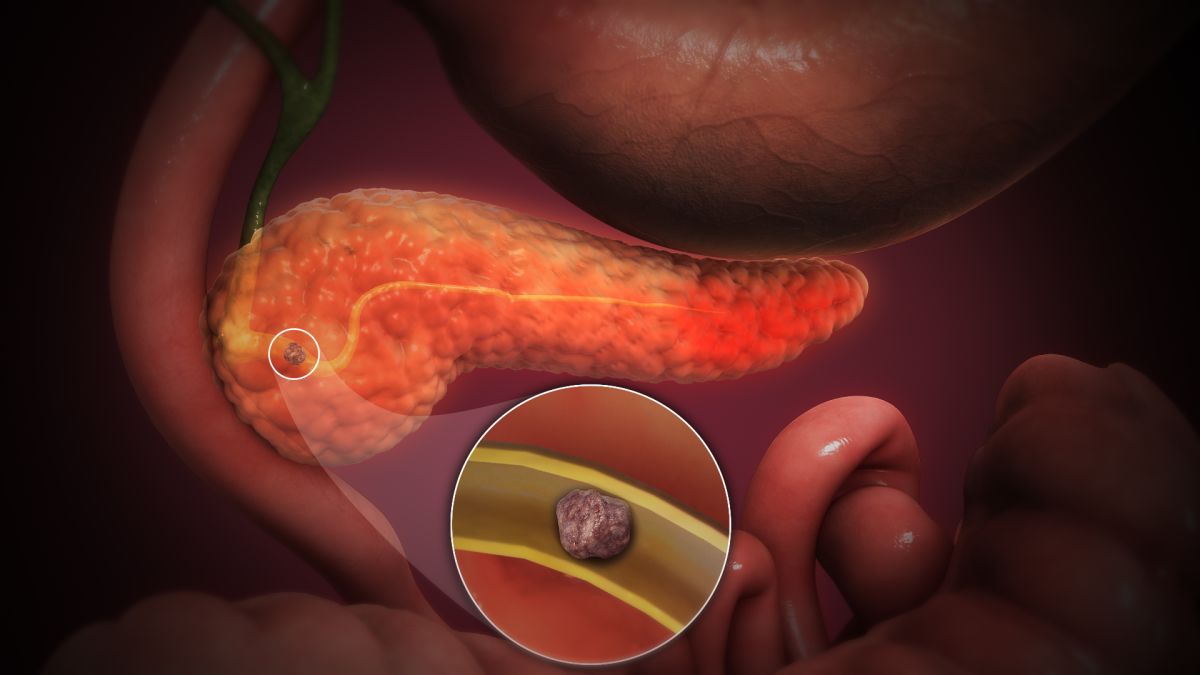
Another proposed cause of acute pancreatitis in pregnancy is high fat levels in the blood called triglycerides. When triglyceride levels become too high, oxygen cannot adequately travel to the pancreas via the bloodstream, and pancreatitis can ensue.
Acute pancreatitis is serious during pregnancy and has been found to be associated with an increased risk of premature delivery, preeclampsia, postpartum hemorrhage, and maternal and fetal death (if not found/treated).
Pancreatitis is diagnosed with lab work and various imaging studies (CT scan, ultrasound, MRI). Pancreatitis results in hospitalization and treatment with IV fluids, pain medicine, and no food or beverages for several days, especially if severe. This allows the pancreas to reduce inflammation and to heal back to normal. Afterward, a low-fat diet is followed for a period of time as determined by an HCP.
If the reason for the pancreatitis is gallstones, removal of the gallbladder may also be completed or a stent can be placed until surgery becomes absolutely necessary.
If the cause of acute pancreatitis is due to triglycerides, certain medications and dietary modifications can be used to help prevent recurrent attacks. However, if the attack occurs late in the third trimester, delivery is usually advocated, as this will cause an immediate decrease in the triglyceride levels.
Benign Masses of the Ovary, Fallopian Tube, and Uterus
Adnexal masses (masses of the ovary, Fallopian tube, or surrounding connective tissues) occur in 2% of all pregnancies, are usually benign, and are most often first detected at the time of a routine ultrasound. It is estimated that only about 35% of these masses cause abdominal pain (most are asymptomatic).
Ultrasound provides the ability to identify adnexal masses that are small, uncomplicated, and likely to resolve on their own from those that appear larger and more complex with a higher likelihood of malignancy. If ultrasound is inconclusive, MRI is often recommended as the next step (no radiation).
The most common adnexal masses during pregnancy are corpus luteum or other ovarian cysts.
Fibroids (leiomyomas) are the most common solid adnexal mass found during pregnancy. “Red degeneration” occurs when a fibroid outgrows its blood supply which results in hemorrhage. It is estimated that 1 in 500 pregnant women are hospitalized for a fibroid-related complication.
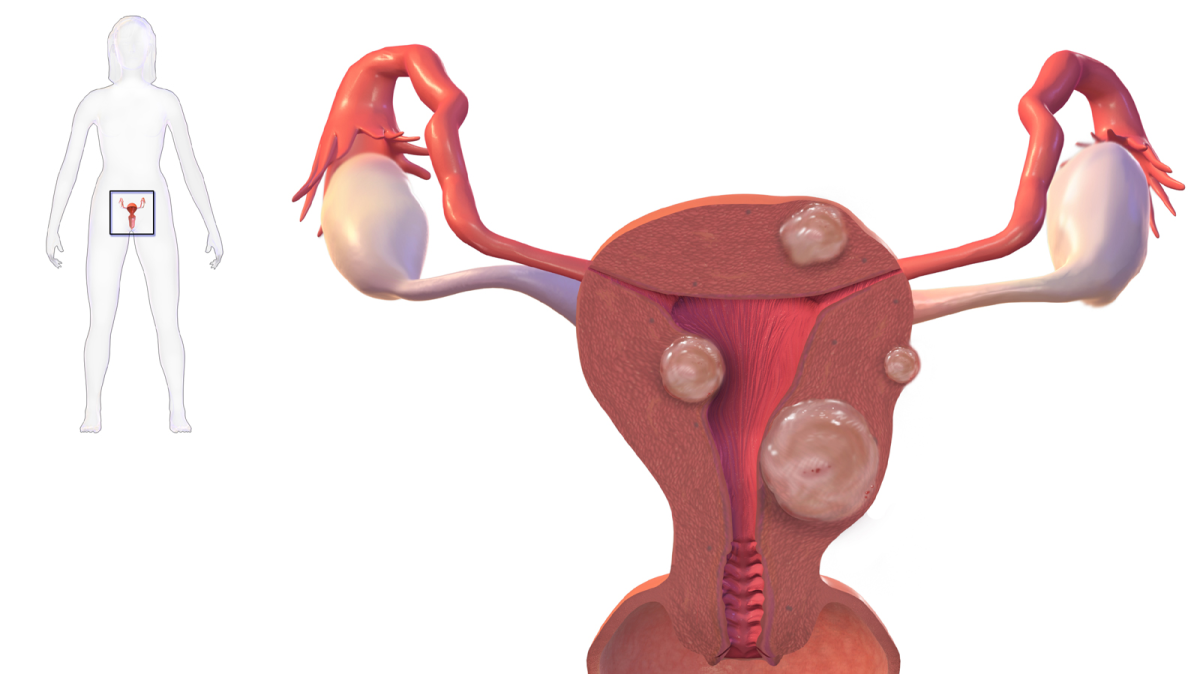
Degeneration (break-down) of fibroids can cause abdominal pain and possibly even contractions.
Approximately half of all fibroids grow during pregnancy, mainly in the first trimester because of rising estrogen levels. The fastest growth rate may occur before 11 to 14 weeks, but this growth may also vary due to multiple factors. While most of this growth cannot be felt, some women can experience abdominal pain.
Subsequent outcomes of pregnancy in women with at least one uterine fibroid are dependent on the number of fibroids present, location, size, and type.
Ovarian torsion (OT) also has an increased incidence during pregnancy. OT diagnosis is difficult, and can involve the tube, ovary, and nearby structures either separately or together, and complicates about 1 in 800 pregnancies during any trimester. Most women with OT present to the emergency room with severe abdominal pain, nausea, and vomiting. These symptoms, especially early in pregnancy, also mirror ectopic pregnancy and hyperemesis gravidarum.
Early diagnosis and laparoscopic surgery is recommended for suspected OT, particularly to save the ovary and surrounding structures for women who wish to preserve their fertility.
Fortunately, a study published in July 2021 indicated that pregnancy outcomes among women who underwent laparoscopy for a suspected adnexal torsion (may also include the Fallopian tube) during pregnancy were reassuring, regardless of surgical findings and gestational week.
Action
Women should always bring abdominal pain (and bleeding) to the attention of their HCP or, if severe, visit the emergency department.
Women should never assume their abdominal pain is a normal result of pregnancy, no matter how unlikely the above conditions may be. Certain conditions such as ectopic pregnancy, preterm labor, and appendicitis are considered emergencies and should be ruled out.
Women should also consider sharing and submitting their experience below regarding abdominal pain during pregnancy. This can help other women understand this concern better and how to talk to their HCP.
Partners/Support
Partners, and other individuals who support pregnant women, can play an important role in the identification of abdominal pain that may require medical assistance. Partners may able to tell when a woman appears to be acting different, or is overly bothered by cramps, pelvic, or abdominal pain.

Some women are very hesitant to call their HCP's office when they experience an issue. Partners can talk women through how they are feeling, and help them understand why calling their HCP or seeking emergency care may be a good idea.
Partners/Support should read the section above to learn about abdominal pain and its possible causes during pregnancy, to be better informed/educated in the event a doctor's/hospital visit is necessary.
Resources
Acute abdomen and abdominal pain in pregnancy (Royal College of Obstetricians and Gynaecologists)
Stomach Pain in Pregnancy (U.K. National Health Service)
If a pregnant woman has experienced physical trauma due to domestic violence, there are numerous resources available to obtain immediate, safe, and discreet medical attention.
Women can:
Call 911.
Call the local police department.
Call the National Domestic Violence Hotline (NDVH) at 1−800−799−7233 or TTY 1−800−787−3224
Go online to thehotline.org (NDVH)
Text LOVEIS to 1-866-331-9474 (NDVH)
Call a close friend or family member who can help the woman collect all necessary belongs and safely leave the residence.