Immune System
NEW: "Postpartum" section added 14 November 2022.
The latest research indicates a pregnant woman’s immune system is not suppressed – it adapts to the pregnancy, allows it to thrive, and does not make a pregnant woman more susceptible to contracting infections. Further, this high activity is necessary for the health of the pregnancy.
However, the adapted immune system, together with lung, heart, and blood volume changes during pregnancy, can make it harder for women to fight off infections (listeria, influenza, etc.) and complications after becoming ill. This is also highly dependent on the type of illness, at which stage of pregnancy a woman becomes ill, and when she receives treatment.
More research is needed to understand the immune system during pregnancy, to include whether the fetus also has an immune system, and which illnesses and infections are consistently more serious during pregnancy.
It is currently assessed the best way to prevent some viral and bacterial infections during pregnancy is for women to get vaccinated (i.e. influenza) and to understand the signs and symptoms of different types of infections to get managed/treated as early as possible.
Background
Theories are constantly evolving regarding the adaptation and function of a woman's immune system during pregnancy.
Researchers learning more about the immune system, whether the fetal/placental unit has its own system, and whether any interaction between the two occurs is critical to better understanding implantation, fetal growth and development, how infections can affect the health of both mother and baby, and how to best treat those infections.
Pregnancy hormones alter the function of immune cells; this alteration can affect the outcome of infections in various parts of the body such as the stomach, intestines, lungs, and genital tract. Exactly how this occurs, and how it affects viral, bacterial, or fungal infections is not known.
Researchers are trying to answer:
How does the woman’s immune system react to pregnancy?
What happens that allows implantation to occur, when the woman’s body should technically reject it?
Does the fetal/placental unit have its own immune system?
Does it interact with the woman’s or is different?
How does the woman’s immune system react to viral/bacterial/fungal infections?
Why are some infections worse at different periods of gestation?
What is the best treatment for pregnant women who contract infections? Should treatment be different depending on stage of pregnancy?
Implantation
Immune cells are present at the sight of implantation. This led to the original hypothesis this was the body's attempt to reject the fetus, and that somehow the fetus was able to successfully implant despite those immune cells.
Part of this theory was based on the fact the fetus has genetic material from someone else (male sperm) and is therefore an invader. Under normal conditions, "invaders" are rejected by an individual's immune system.
The immune cells at the implantation site were assessed to be "weaker" to allow for implantation, leading to the overall assessment that pregnant women have a weakened immune system throughout gestation; however, the latest research points to a reversal in this hypothesis.

It is now believed the significant presence of the woman’s immune cells at the implantation site (i.e. an inflammatory reaction), is not a response to a “foreign invader” as previously believed but a response to assist in its growth and development.
A study published in July 2021 indicated researchers may have identified the subset of immune cells that are needed so the mother's body does not "reject" the early pregnancy. This subset of cells "teaches" the rest of the immune system to tolerate the pregnancy and allow it to grow and develop.
Therefore, the mother’s immune system is not only quite active at the implantation site, but its high activity is necessary for successful implantation. It is currently theorized the fetal/placental unit also has its own immune system, which works together with the mother's, instead of against it (however, more research is necessary).
This is further evidenced by the negative effects that occur due to removal of immune cells at the implantation site. If the previous theory was correct, then nothing would happen – in fact, removal would be helpful; but when these cells are depleted/removed, trophoblast cells cannot reach deep into the uterine wall and implantation is unsuccessful (i.e. the inflammation caused by those immune cells helps the embryo implant).
Inflammatory State
Early pregnancy is therefore considered a pro-inflammatory state, followed by a significant amount of gestation at an anti-inflammatory state (or “tightly controlled inflammation”). The body returns to a pro-inflammatory state again near term to initiate labor.
The second immunological phase of pregnancy (anti-inflammatory) is considered the “optimal time” for pregnant women, as nausea and vomiting goes away, women have more energy, and there is rapid fetal growth and development. Further, this phase promotes an increase in the transfer of maternal antibodies to the fetus.
Labor and delivery are characterized by a significant increase of immune cells back into the uterus to revert to a pro-inflammatory process again to initiate contractions, deliver the baby, and detach the placenta. It is theorized that preterm labor by the result of the body reverting to this inflammatory process too early (i.e. due to infection, one of the leading causes of preterm delivery).
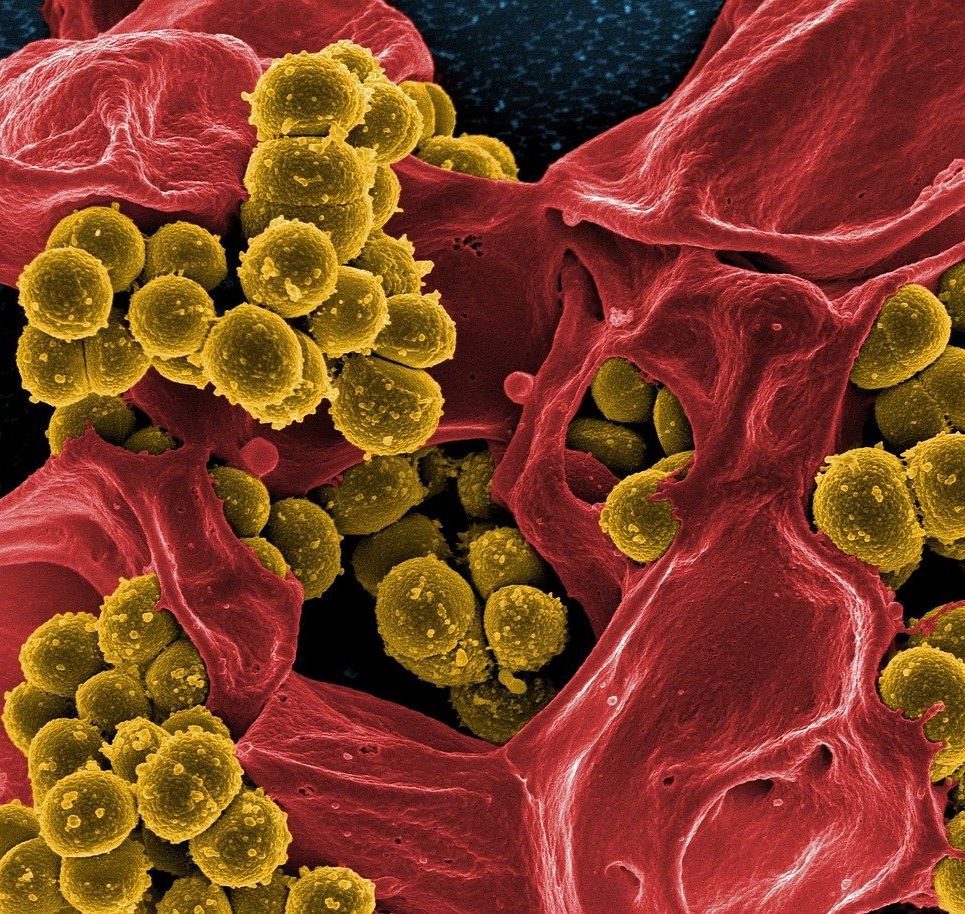
Infection
Based on the above, pregnant women are not necessarily more vulnerable to contracting infections any more than non-pregnant individuals. However, it is possible that women may experience more complications after becoming ill.
A pregnant woman’s immune system reacts differently to microorganisms due to its altered function and varied inflammatory states.
The severity of any particular illness during pregnancy likely depends on the type of infection (bacterial, viral, fungal), the stage of pregnancy a woman becomes ill, the extent of the inflammatory response to the infection, whether the disease spreads to the fetus, and the overall health of the woman.
Because most of pregnancy can be considered an anti-inflammatory state, in general, women with inflammatory conditions during pregnancy (multiple sclerosis, psoriasis, rheumatoid arthritis) get better during pregnancy, and women who contract viral infections requiring an inflammatory response tend to get more severe infections (influenza, STDs).
However, the anti-inflammatory state for most of pregnancy prevents or slows down an inflammatory response to viruses such as the flu, but the inflammatory response is necessary to combat and prevent it from spreading quickly through the body.
Certain infections can also cause the immune system to overreact:
A 2012 study found an unusually strong hyperinflammatory reaction to the flu virus during pregnancy, meaning the immune system overreacted, creating a “super inflammatory state” (cytokine storm). This response could be the theoretical cause of why the flu during pregnancy sometimes leads to severe lung inflammation and preterm birth (which is initiated by severe inflammation).
A September 2020 study studying pregnancy and the flu added weight to the above. The [animal] study suggested the flu virus does not stay in the lungs but spreads throughout the mother's body through the blood vessels and into the circulatory system, triggering a damaging "hyperactive" immune response. The study authors noted this goes against the "suppressed" immune system theory.
It is possible that certain viral infections such as influenza put the immune system of a pregnant women into such disarray by essentially “reversing” the immunological state it needs to be in, in order to maintain a healthy pregnancy.
Note: Regarding COVID-19, pregnant women are not more susceptible to contracting the illness more than non-pregnant women. However, they are more likely to experience certain complications. Read more.
Fetal Transmission
Most viral infections affecting pregnant women rarely cause fetal infection during pregnancy (but can be passed during vaginal delivery), which is not true of bacterial or fungal infections, which can spread to the fetus during pregnancy (syphilis, oral/genital herpes).
If bacteria reach the uterine lining (urinary tract infection/lower genital infections), a pro-inflammatory response is induced that can negatively affect pregnancy outcome. This occurs through the initiation of contractions, leading to preterm birth, or inflammation that disrupts fetal development.
Additionally, if a pregnant woman already has a viral infection, the placenta then becomes hypersensitive to bacterial infection, and both types of infection together can induce an inflammatory response which could very likely result in preterm birth.
Postpartum
Compared to during pregnancy, the "postpartum immune system" is even less understood. Current evidence indicates it could take, on average, 2 to 4 months for the immune system to return to its pre-pregnancy state. However, this could take as long as 12 months depending on lactation status and other factors.
The postpartum state includes childbirth recovery, lactation processes, a return to a regular menstrual cycle, and hormone regulation. All these variables are highly individualized.
Current infections that may affect postpartum women at a higher rate appear to include endometritis, urinary tract infections, and wound infections. It also appears that postpartum women may be at a higher risk of severe COVID-19 infection, but this is not as well-defined as the risk during pregnancy.

Action
This unique immunological state can make it very difficult to treat pregnant women who contract an infection and research remains ongoing.
Women who believe they may have an infection need to call their health care provider immediately, especially if fever is also present.
It is currently assessed the best way to prevent some viral and bacterial infections during pregnancy is for women to get vaccinated (i.e. influenza) and to understand the signs and symptoms of different types of infections to get managed/treated as early as possible.
Women should read more information regarding vaginal infections, urinary tract infections, fever, listeria, syphilis, oral/genital herpes, and respiratory infections, including influenza and COVID-19.
Resources
Overview of the Immune System (National Institute of Allergy and Infectious Diseases)