Teeth and Gums

Pregnancy causes changes to the gingiva (gums) during pregnancy that can negatively affect the health of the entire mouth without proper care.
Bacteria involved in periodontal disease have been found in amniotic fluid. These pathogens could spread to the blood stream and enter the placenta, potentially triggering an inflammatory response that could to lead to preterm delivery or other negative outcome (read below for more information).
Routine dental appointments are important for optimal oral health and the prevention of gingivitis, periodontal disease, and the possible complications caused by these conditions during pregnancy.
Women should continue reading to find out why pregnancy has such an effect on the mouth and what actions they can take to prevent problems. If pregnant women have any questions or concerns regarding their oral health, they should call their dentist.
Background
Pregnancy directly affects the mouth, and this association has been formally documented since as early as 1877. Further, the identification of the different mechanisms for how this occurs and what hormones are responsible has greatly improved since then.
One of the earliest theories in "oral-obstetric" health was that pregnant women lose "a tooth for a child" due to calcium loss from their teeth and bones to support the fetus. Current research shows if a woman is deficient in calcium, it is likely only her bones will deplete of calcium – not her teeth (the bones eventually recover).
However, tooth damage can occur during pregnancy as a result of gum-related changes that impact the teeth:
Estrogen and progesterone levels increase significantly during pregnancy, and receptors for these hormones are found in the gingiva (gums) which means these hormones directly affect the entire mouth, even in women with good oral hygiene.
The most commonly seen oral changes during pregnancy are gingivitis, periodontal disease, slight tooth mobility, pyogenic granuloma, mouth sores, and excess saliva. It is unclear if pregnancy itself increases the risk of cavities (caries).
Gingivitis
Pregnancy gingivitis (inflamed, bleeding, sore gums) is considered the most common oral-related condition during pregnancy, occurring in 60% to 100% of pregnant women.
In non-pregnant individuals, gingivitis is normally caused by plaque. This does not appear to be the cause during pregnancy, as gingivitis still occurs in pregnant women who have excellent oral hygiene before and during pregnancy (and therefore, very little plaque).
It is assessed that hormones cause the increased blood vessels in the mouth to overreact to any plaque/bacteria, leading to significant inflammation that causes bleeding and soreness, regardless of plaque levels; progesterone also favors the growth of bacteria.
The progression and peak of gingivitis in pregnancy is debated, but it likely gets worse as pregnancy continues, thereby peaking in the third trimester. However, there does appear to be a marked decrease in gingivitis in the last month of pregnancy as hormone levels begin to drop in preparation for labor.
Gingivitis may irritate the gums to such an extent that brushing and flossing are too painful for women to achieve even once per day, which could further lead to cavities and/or periodontal disease.
Fortunately, the symptoms of gingivitis disappear almost immediately after delivery, indicating that the condition is reversible in the postpartum period.

Periodontal Disease
Periodontal disease (PD) – chronic inflammation of the gums due to bacteria – usually follows gingivitis when not treated. Therefore, gingivitis can technically be called the earliest form of PD. Pregnancy can also worsen the condition if it existed in a woman prior to pregnancy. Fortunately, PD does appear to improve after delivery in women with proper oral hygiene.
The increased levels of relaxin during pregnancy can lead to tooth mobility. This tooth mobility, together with any untreated cavities, can also lead to PD due to inflammation and irritation of the periodontal ligament. Loose teeth is also a symptom of PD.
Although the cause of PD is not directly pregnancy-related (but gingivitis is), PD does affect outcomes of pregnancy by causing abnormal immunologic changes.
Bacteria involved in periodontal disease have been found in amniotic fluid. It is possible that these pathogens can travel through the blood stream, enter the placenta, and stimulate an inflammatory response which could lead to miscarriage, preterm labor, or preeclampsia.
Bacteria involved in periodontal disease has been found in amniotic fluid, stressing the importance of practicing good oral hygiene and having at least one routine dental appointment during pregnancy.
It is estimated that up to 18 of every 100 premature births may be triggered by PD, and that pregnant women with PD may potentially be seven times more likely to deliver preterm, especially if the woman’s PD worsened during pregnancy.
Researchers currently advocate for further investigation regarding how a woman's oral microbiome can affect her pregnancy. (Note: Researchers are also assessing how a woman's vaginal microbiome can do the same).
However, the causes of preterm delivery are complex, and not all studies have found an association between PD and preterm delivery. Further, numerous studies found no reduction in preterm delivery risk even when PD was treated during pregnancy.
It may be possible that treatment could be too late to reduce risk once PD is present. This would further illustrate the need for good oral health prior to and during pregnancy.
One systematic review, however, did indicate a significant reduction in risk when scaling and root planning occurred during pregnancy, which is an intense cleaning of the gum line by a dentist (this procedure is considered safe during pregnancy, see below).
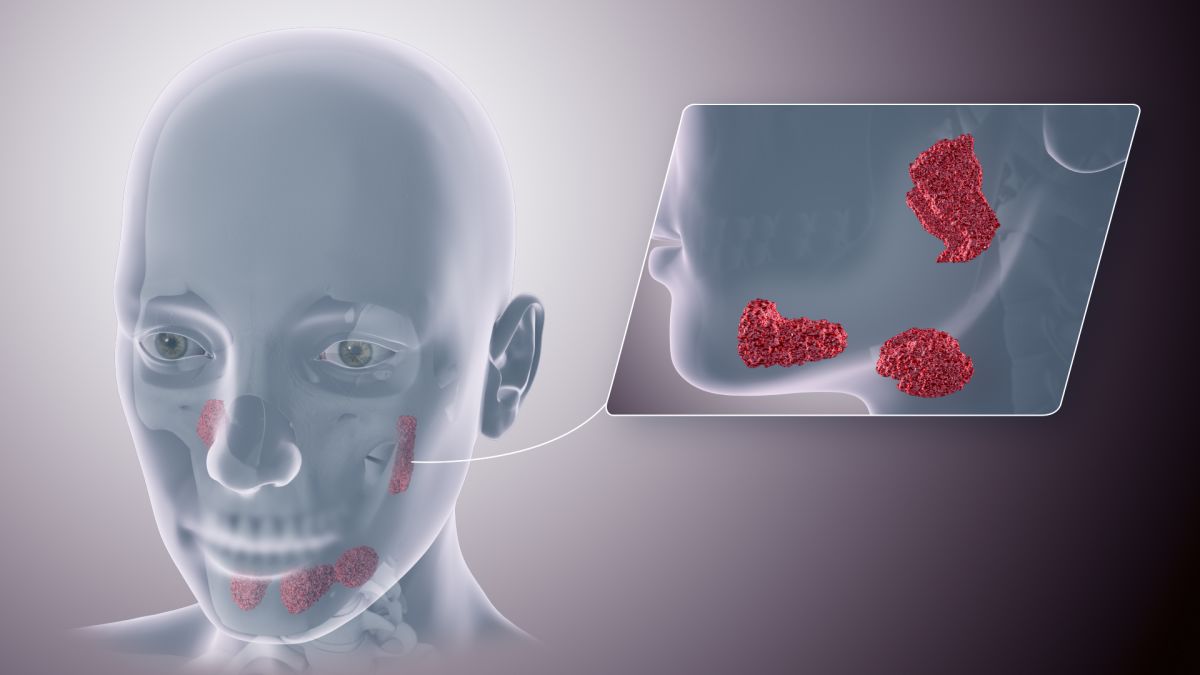
Granulomas
A pyogenic granuloma is a localized, bright red, soft lesion in the mouth that may also have small white flecks. It may easily bleed when touched, measure up to 2 centimeters, and continue to grow throughout pregnancy. Large granulomas may even cover part of a tooth. They usually heal after delivery.
Pyogenic granulomas occur in up to 9% of pregnant women and appear to be most common in early pregnancy. They are likely caused by increased blood vessels, inflammation, and plaque.
If severe, pyogenic granulomas can be removed through oral surgery. Although safe during pregnancy, the procedure carries a risk the granuloma may quickly return before delivery.
Example: Image 1
Saliva
The main changes to saliva during pregnancy involve flow, composition, pH, and hormone levels.
Excessive saliva during pregnancy, known as ptyalism gravidarum, is rare and does not cause serious complications during pregnancy, but there is also no treatment or good method for symptom control. Symptoms may subside late in the third trimester or after delivery, when hormone levels drop or return to normal.
It is generally agreed that stimulation of the nerve supply of the salivary gland during pregnancy causes the gland to produce excess diluted saliva that closely resembles water.
Excessive saliva is common in women with nausea and vomiting of pregnancy (NVP) and was previously strictly associated with women who suffered from hyperemesis gravidarum. Women may have difficulty swallowing the excess and need to spit it out frequently, exacerbating NVP.
Ptyalism may also make sleeping difficult and day-to-day employment and social activities hard to manage. Unfortunately there is very little information on this symptom during pregnancy.
Appointments, Procedures, and Medications
It is recommended women see their dentist at least once during pregnancy to treat and prevent possible complications. However, a study of 75,876 women between 2012 and 2015 determined that:
Only 51.7% reported they had at least 1 dental visit for cleaning during their most recent pregnancy.
One of 5 (19.7%) experienced dental problems during pregnancy, but 34.4% of these women did not visit dentists to address the problems.
Routine cleaning appointments are safe during pregnancy, and dental hygienists and dentists can be more gentle/sensitive while cleaning due to the likelihood of sore and bleeding gums.
Dentists may follow a standard rule of recommending any dental procedure (other than cleanings) for the second trimester or later, even when the risk of a procedure on the mother or the fetus is considered negligible.
Some extensive and prolonged dental procedures may be postponed until after delivery unless deemed necessary by an HCP (and the patient).
Conditions that require immediate treatment, such as trauma, extractions, root canals, and restoration of untreated cavities may need to be performed during the first trimester. Delaying treatment may result in more complicated problems and pregnant women should discuss all potential forms of treatment, time frames, and risks and benefits with their HCP.
Some research indicates scaling and root planning are safe for any stage of pregnancy, to include the first trimester, which may be necessary to assist in the treatment of PD.
Pregnant women should lie comfortably in the dental exam chair during any exam, cleaning, or procedure to avoid vena cava syndrome while in the horizontal position. Women should also keep their right hips slightly raised (10 to 12 cm) with a slight tilt to the left side, which further reduces potential discomfort.

Local anesthetics such as lidocaine and prilocaine are considered safe when administered properly, and have not been linked to any negative complications of pregnancy.
Fillings (for cavities) are also safe during pregnancy, but silver amalgam fillings containing mercury should be avoided – even if the risk is low – due to viable alternatives.
Composite resin (tooth-colored) is a filling option without the potential mercury risk but does cost more and does not last as long. It is not recommended to remove or replace previous fillings that contain mercury until after pregnancy. Women should discuss all their options with their HCP.
Fluoride supplements are not recommended during pregnancy due to the potential lack of effectiveness and are recommended during the postpartum period if needed. Fluoride in toothpaste is safe and recommended during pregnancy.
Dental X-Rays
Unless necessary due to significant trauma or risk of infection, HCPs will usually wait until after delivery to take dental X-rays even though most X-rays do not affect the abdomen or pelvic area.
If a pregnant woman and her HCP determine X-rays are required, the radiation risk to the fetus is considered extremely low, especially when additional precautionary measures are taken. A leaded apron should be used to shield the abdomen, a thyroid collar should be placed around the neck, and speed films should be used.
The volume of radiation that a fetus may acquire from a mother’s dental X-ray is only 0.01 millirads.
The mother would need 100,000 dental X-rays for the fetus to receive just 1 rad.
The reported dose of radiation to result in an increased incidence of birth defects or miscarriage is more than 20 rads, or more than 2,000,000 million dental X-rays.
Read Radiation for more detailed information.
Action
Women should always contact their dentist when experiencing bad breath, sore and bleeding gums, loose teeth, mouth sores or other growths, and tooth and gum pain, as well as for regular cleanings during pregnancy. Dentists may also recommend prescription toothpastes or fluoride rinses, which are safe when used properly during pregnancy.
Pregnant women need to inform their dentist of their pregnancy prior to their appointment or procedure.
To help prevent tooth decay, gum disease, and any potential oral health related complications during pregnancy, women should stop smoking and vaping, brush teeth thoroughly at least twice a day, floss, and have regular check-ups to include at least one before and during pregnancy. Note: Every three months during pregnancy is ideal, especially with preexisting disease.
Women should use a soft bristled brush when possible to avoid further irritation/soreness to the gums.
Women who are afraid or anxious to visit a dentist should talk to their HCP or a family member who can offer support. Some dental offices allow women to tour, meet several members of their staff, and answer any questions regarding potential fears or concerns.

Delaying appointments/treatment may result in more complicated problems, and pregnant women should discuss all potential forms of treatment, time frames, and risks and benefits with their HCP.
Read more information regarding maintaining proper oral health when experiencing nausea and vomiting of pregnancy.
Partner/Support
Partners/support can help women maintain good oral health during pregnancy by:
Attending appointments with her if she is too anxious or nervous
Helping her brush her teeth when she is suffering through NVP by getting a variety of flavors and types of mouthwash and toothpaste (gel, paste, foam) and different styles of toothbrushes, and making sure baking soda is also available (read more)
Eating healthy so that she eats healthy as well, by avoiding excess sugar as much as possible which can exacerbate tooth and gum health, especially if she is having trouble brushing.
Avoid/quit smoking and/or vaping around her if she is trying to do the same. Partners who quite smoking can greatly improve not only their health, but the health of the woman and baby as well (read more).
Gaps
Should women who are diagnosed with periodontal disease during pregnancy be routinely monitored for preterm labor similar to other women considered high risk for preterm labor?
Resources
Oral Health and Pregnancy (European Federation of Periodontology)
Types of Gum Disease (American Academy of Periodontology)