Gastrointestinal Tract
Hormones have a significant effect on the gastrointestinal (GI) tract, which includes slowing it down, impeding it, or changing its regular pattern of digestion.
It is assessed that progesterone’s relaxation effect on gastric motility likely causes food to stay in the GI tract longer, leading to various symptoms such as nausea, vomiting, acid reflux, heartburn, constipation, and hemorrhoids.
However, researchers do not completely understand the full hormonal effects on the GI tract, to include whether motility is truly affected – and if it is – to what degree it is affected, and whether those changes are the cause of certain symptoms.
For example, while some researchers have found motility to slow down during pregnancy, others have noticed no change at all, except during labor.
Therefore, it is possible that women with moderate to severe GI symptoms may experience more of an effect from progesterone than others, but critical gaps remain as research remains inconsistent.
Women should also read Causes and Contributing Factors of Nausea and Vomiting of Pregnancy for more information.
Background
Gastrointestinal (GI) changes during pregnancy create many significant symptoms. Pregnant women routinely experience nausea, vomiting, acid reflux, heartburn, constipation, and hemorrhoids.
Fortunately, most of these concerns are considered short-term and easy to control with dietary or lifestyle modifications and/or medication.
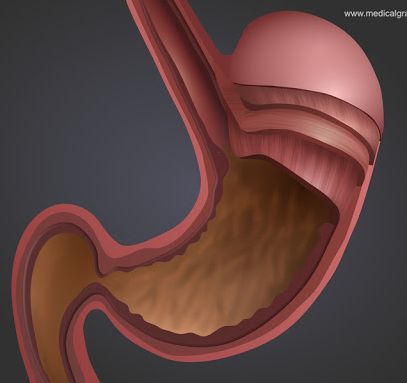
The most significant change to the GI tract appears to be on motility. "Motility" is a term used to describe the contraction of the muscles that mix and push contents into the GI tract.
However, although these changes are considered relatively impactful, researchers do not yet have a full or complete understanding of motility changes during pregnancy.

Motility and Transit Time
It is largely believed that progesterone inhibits the ability of the stomach and intestines to contract; therefore they “move” slower, and food remains in the GI tract longer.
The is one of the most commonly stated causes of nausea and vomiting of pregnancy.
It is theorized the "purpose" of this slower digestion allows for maximum absorption of vitamins and minerals, although it also leads to nausea, reflux, and constipation as a result.
However, even though commonly cited, evidence is inconsistent regarding GI tract motility during pregnancy, and rate of emptying has only been partially studied. Part of this inconsistency is due to the limited methods researchers can use to measure emptying time, as the most accurate imaging techniques use radiation.
Note: These gaps are critical, as understanding this information could affect the type, dosage, and efficacy of medications prescribed during pregnancy. Rate of gastric emptying can affect how medication is absorbed by the body.
Other studies have documented no change in GI tract motility at any stage during pregnancy, although a few indicated labor does appear to cause a definitive “slow down”.

Concern over food in the GI tract during labor is one of the main drivers of the fasting (no food) rule during labor and delivery, although even this rule has relaxed in most practices in recent years.
It is possible, that women with moderate to severe GI symptoms during pregnancy may be more affected by progesterone’s effects on motility than women without these symptoms. For example, at least one study showed women with hyperemesis gravidarum (HG) demonstrating prolonged gastric emptying in comparison to those without HG.
Dysrhythmias
While motility remains debated, it does appear some women can experience stomach dysrhythmias during pregnancy that can worsen early pregnancy symptoms.
The stomach possesses pacemaker tissue (like the heart) which generates slow wave-like motions with set consistency. Dysrhythmias are disturbances of this pattern, either faster or slower, that are present in some women with NVP .
Progesterone and estrogen likely cause this disruption of the stomach, as researchers were able to replicate dysrhythmias by administering to non-pregnant women either progesterone, or in combination with estradiol, in doses equal to pregnancy levels.
Vasopressin also induces gastric dysrhythmias, which leads to nausea and vomiting in non-pregnant individuals. Vasopressin is increased in early pregnancy due to an increase in HCG that allows for the normal physiological changes associated with pregnancy.
However, the exact causal relationship between gastric dysrhythmias and motility of the GI tract are not understood.
Resulting Effects
Constipation is second only to nausea as the most common gastrointestinal complaint in pregnancy. Constipation usually occurs in the first and second trimesters, affecting up to 40% of women.
Elevated levels of progesterone and relaxin may work together to cause food to move slower through the digestive tract. Even if motility is debated, any slight effect on motility can increase water absorption in the colon, leading to dry and hard stool that is difficult to pass.
Constipation leads directly to hemorrhoids during pregnancy due to prolonged straining. Hemorrhoids occur when the external veins near and around the rectum become enlarged and swollen, causing itching, burning, painful bowel movements, and/or bleeding.
The prevalence of hemorrhoids in pregnant women ranges from 25% to 85%. This large range is likely due to hesitation by pregnant women to report this symptom.
Progesterone and relaxin are likely also responsible for the relaxation of the valve between the stomach and esophagus (lower esophageal sphincter), which makes it easier for acid to travel back up the esophagus. This, on top of the possible delay in gastric emptying, causes many pregnant women to experience acid reflux and heartburn symptoms.

Further, later in pregnancy, the upward movement of the uterus and other internal organs increases intra-abdominal pressure which worsens these symptoms.
Nausea and vomiting of pregnancy (NVP) has many possible causes and is likely due to more than one occurring simultaneously, especially in those with severe NVP. While motility and other GI tract changes likely play a role, other causes of NVP may not lie within the GI tract (read more).
Action
Gastrointestinal symptoms can be difficult to manage during pregnancy, especially nausea and vomiting. Women should not be afraid (or embarrassed) to explain their symptoms to their HCP, as there are many management options and strategies to help women cope with these symptoms.
Further, many women can find relief with lifestyle and dietary changes – or if severe – with over-the-counter or prescription medications) as recommended by their HCP).
Women should never take any supplement or over-the-counter medication during pregnancy without speaking to their HCP first.
Women should also consider reading the following additional topic pages for more detailed information:
Gaps
If motility is theorized to potentially play a major role in GI symptoms, then why do women still feel ill after eating small meals, or even only fluids?
Resources
Your Digestive System and How it Works (The National Institute of Diabetes and Digestive and Kidney Diseases)