Hemorrhoids

Hemorrhoids are swollen veins in and around the rectal/anal area caused by various pregnancy-related causes such as poor lower body circulation, constipation, and swelling.
Despite the fact most women avoid talking about them, hemorrhoids are one of the most common medical problems in the general population and there are various options available for managing symptoms.
Women should tell their HCP if they believe they have symptomatic hemorrhoids. HCPs can recommend best prevention practices and ask a few questions to potentially rule out other conditions that could be causing the same symptoms.
Background
Constipation is second only to nausea as the most common gastrointestinal complaint in pregnancy. This can lead directly to hemorrhoids (also known as piles) due to prolonged straining that occurs when an individual is constipated.
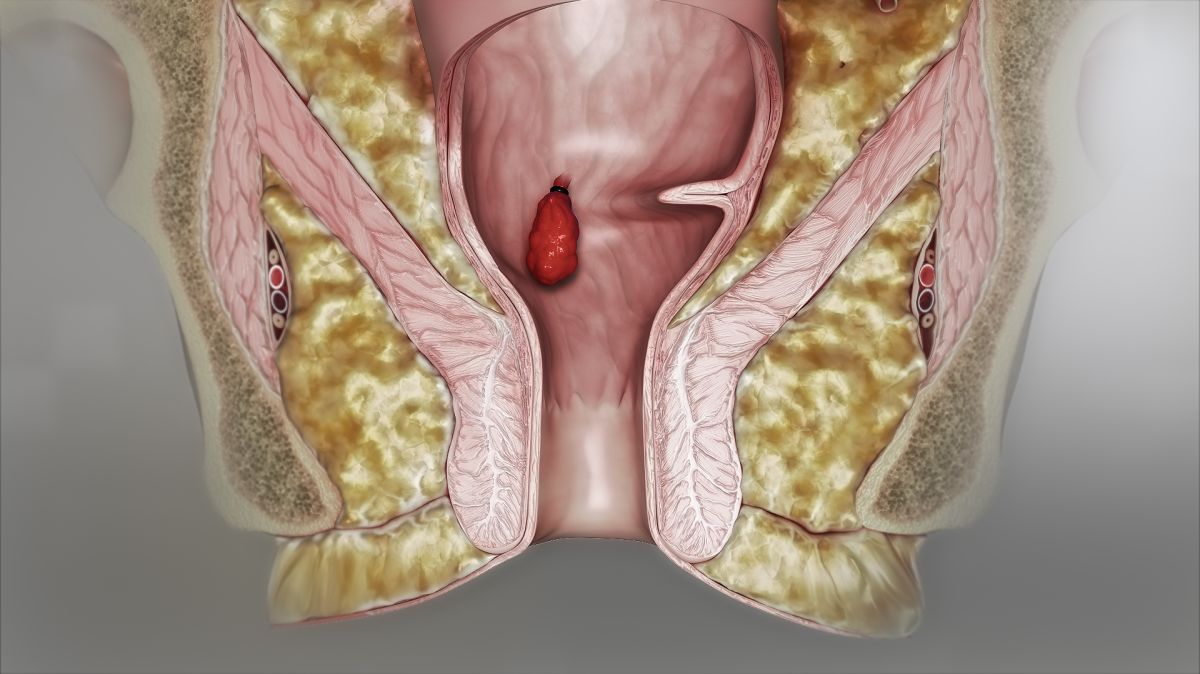
Hemorrhoids occur when the external veins near and around the rectum become enlarged and swollen, causing itching, burning, painful bowel movements, and bleeding.
Hemorrhoids is recognized as one of the most common medical conditions in general population and is a top trending health issue in the United States. The prevalence of hemorrhoids in pregnant women ranges from 25% to 85%; this large range is likely due to hesitation by pregnant women to report this symptom.

Pregnancy-induced Causes
Hemorrhoids are very common during pregnancy especially in the third trimester, due to the increased weight of the uterus which puts pressure on the pelvic, vaginal, rectal, and anal blood vessels; these vessels then become swollen.
Although there is a lack of strong evidence, additional contributory factors may include lack of dietary fiber, prolonged straining, heavy lifting, spending excess time on the toilet, diarrhea (through irritation), lack of physical activity, and family history.
Signs and Symptoms
Hemorrhoids can be either internal or external, and usually cause painless bleeding along with swelling, discomfort, discharge, hygiene problems, soiling, itchiness, and/or pain with bowel movements. They can affect every aspect of a woman’s life from sitting comfortably, using the bathroom comfortably, to walking, working, and picking up and playing with kids.
While bleeding is a sign of hemorrhoids, it is very specific. The blood is normally bright red and is not mixed in with stool, but coated on the outside of the stool and can be seen on toilet paper after cleaning. There may also be several drops of blood that follow afterward. Pain that accompanies bowel movements is usually due to fissures/tears in the anus due to constipation or heavy straining.
Blood that is mixed with stool, is darker, occurs without bowel movements, or if severe pain is also present, needs immediate further assessment for potential other causes.
A lump hanging outside the anus indicates a prolapsed hemorrhoid, and it may need to be pushed back in after a bowel movement. Prolapse is more likely to occur in women who had hemorrhoids prior to pregnancy.
Most symptoms from hemorrhoids go away postpartum as their causes (uterine weight, constipation) are relieved after delivery.
Severity
Hemorrhoids are classified by severity through degrees or grades:
Grade I: Bleed but do not prolapse
Grade II: Prolapse during a bowel movement but return/regress on their own
Grades I and II can be treated with medical treatment or office procedures.
Grade III: Prolapse but require manual reduction (pushing them back in)
Grade IV: Prolapse and do not return or regress, even with manual attempts/remain outside the anal canal
For Grades III-IV, women should have an individualized treatment plan that may include surgical treatment.

Women are often afraid to mention their symptoms to their HCP because of embarrassment and/or concern over a potential physical exam by the HCP of the anal area. However, this physical exam is important to rule out any other more potentially serious causes and to determine an effective method of treatment. Fortunately, mild hemorrhoids gradually resolve after delivery, and in some cases, no treatment is required.
Management – Lifestyle
Since most hemorrhoids resolved after delivery, a primary goal of treatment is to relieve symptoms and avoid worsened severity through dietary and lifestyle modifications.
First – women should increase fiber in the diet through foods or supplementation with plenty of water to help relieve any constipation that can cause straining; women should also get physically active which improves digestion and blood flow. The avoidance of long periods of sitting or standing can also help.
Women generally find relieve through a warm bath (or sitz bath), but without the use of harsh soaps or other bath products (bath bombs may irritate the anus or vagina).
Witch hazel (an astringent) medicated pads can be applied to the anal area and are commonly given to women to use in the hospital immediately after delivery and to take home. Women can also try ice cold cloths to gently dab to help ease pain.
Lying on the left side can also provide temporary relief by relieve swelling and pressure due to the uterus pressing on the inferior vena cava (vein from the pelvis to the heart).
After passing stool, women should clean with wet wipes instead of toilet paper and pat dry.
If women experience hemorrhoids that prolapse and need to be pushed in, women should call their HCP if they are uncomfortable doing this themselves or are unsure how to do it; they can usually be pushed back in gently with a clean, lubricated finger.
Management – Medication
Various topical creams and ointments are often recommended to pregnant women with hemorrhoids despite a lack of evidence regarding effectiveness – although their use appears to be safe during pregnancy.
Topical medications usually have anti-inflammatory and pain-relieving properties that provide short-term relief from itching, pain, discomfort, and bleeding.
Oral phlebotonic flavonoid drugs are also sometimes used for treatment of hemorrhoids during pregnancy in several countries. These drugs decrease the fragility of capillaries and can improve circulation. Currently, the U.S. Food and Drug Administration does not approve the use of micronized, purified flavonoid fraction in the United States.
Management – Medical/Surgical
Medical/Surgical techniques for the management of hemorrhoids includes rubber-band ligation, sclerotherapy, infrared coagulation, bipolar diathermy and direct-current electrotherapy, cryotherapy, and laser therapy.
Rubber Band Ligation is the most popular non-surgical, minimally invasive technique for Grades I to III hemorrhoids that do not respond to lifestyle or topical management. It involves placing a rubber band around the hemorrhoid to restrict its blood supply. It represents about 80% of all procedures and has high success and low complication rates.
Hemorrhoidectomy, complete removal of a hemorrhoid, is also an option but is generally saved for the most severe cases of thrombosed hemorrhoids.
Action
Women should talk to their HCP if they believe they are suffering from hemorrhoids and want to discuss possible symptom relief.
Women should also try the lifestyle/diet modifications described above, after talking with their HCP.
If women are too nervous to bring up this topic to their HCP, they should consider emailing their HCP this article, so the HCP knows to bring it up first to make the conversation easier.
Women should also consider sharing and submitting their experience below regarding hemorrhoids during pregnancy. This can help other women learn additional perspectives regarding this concern, how to potentially manage symptoms, and how to talk to their HCP.
Resources
Problems of the Digestive System (American College of Obstetricians and Gynecologists; January 2014)
The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Hemorrhoids (2018) *not specific to pregnancy but some aspects may be applicable to pregnancy