Heartburn and Acid Reflux

Acid reflux is common during pregnancy in all trimesters and can begin very early. Reflux is the “event” that causes the “burning” in the chest known as heartburn. Reflux can also cause nausea and vomiting, a sore throat, coughing at night, increased aversions to foods, and irritation of the gag reflex.
Some women with nausea and vomiting of pregnancy could be unknowingly experiencing severe reflux they are attributing to other causes. This is critical, as reflux can be safely treated during pregnancy through lifestyle modifications, dietary changes, and medications such as antacids, antihistamines, and/or proton pump inhibitors.
Heartburn can be treated the same way, which is mostly felt during the third trimester as the uterus grows out of the pelvic cavity and begins to put pressure on anything above it.
Women should read below for more detailed information on the causes of reflux and heartburn symptoms, as well as lifestyle/diet modifications and medications that can be used to manage discomfort. Women should also talk to their health care provider (HCP) if they have any questions.
Background
Heartburn is a very common and synonymous symptom during pregnancy; up to 80% of women may experience it at some point during pregnancy.
The cause of heartburn is acid reflux. Acid reflux can occur at anytime during pregnancy, although most women feel its resulting heartburn more often in the third trimester.
Reflux does not always present with heartburn, therefore some women may not even realize they are experiencing acid reflux during pregnancy if they are only expected the heartburn symptom.
Acid reflux (the cause): stomach acid overflowing into the esophagus, resulting in heartburn; in medicine, reflux generally means “in a direction opposite to normal” (i.e. acid traveling back up from the stomach).
Heartburn (the symptom): stomach acid that touches the lining of the esophagus can cause heartburn, also called acid indigestion; felt as a burning sensation in the chest
Other signs and symptoms can include difficulty swallowing, coughing, wheezing, nausea, vomiting, and chest pain — especially while lying down at night.
Note: Acid reflux is a common cause of chronic cough during pregnancy, without noticeable heartburn. It is advised if pregnant women frequently cough at night, or have a cough with no other symptoms of a cold, to call their HCP for an assessment and inquire about acid reflux as a possible cause.

Causes, Symptoms, and Long-Term Effects
Heartburn and reflux are documented to occur in 50% to 90% of all pregnancies with varying degrees of severity throughout all trimesters.
The upper gastrointestinal (GI) tract is greatly affected during pregnancy. It is currently believed (but debated) that progesterone inhibits the ability of the stomach and intestines to contract; therefore they “move” slower, and food remains in the GI tract longer.
Further, relaxation of the valve/sphincter between the stomach and esophagus due to progesterone and relaxin makes it easier for acid to travel back up the esophagus. This, on top of the possible delay in gastric emptying, can make most women experience reflux and heartburn symptoms during pregnancy.
It is also possible that women with moderate to severe GI symptoms during pregnancy may be more impacted by hormonal effects on the upper GI tract than women without these symptoms.

Later in pregnancy, the upward movement of the uterus and other internal organs increases pressure and shifts organs up. This is the likely cause of the higher prevalence of women feeling heartburn later in pregnancy.
Reflux symptoms can range from mild to severe as early as the first trimester. Therefore, it is assessed that reflux that occurs early in pregnancy can cause, contribute to, or exacerbate nausea and vomiting of pregnancy. Women may not recognize this as a possible contributor because they may not be feeling the tell-tale sign of heartburn. Further, reflux can cause nausea and vomiting in non-pregnant individuals.
Additionally, reflux can cause foods to taste differently, exacerbating aversions that can lead to nausea. It can also lead to irritation of the upper esophagus and more easily trigger the gag reflex leading to gagging and/or vomiting. However, reflux appears to most significantly impact the ability to sleep.

For most women, reflux symptoms disappear postpartum, as hormone levels return to normal and the uterus shrinks back into the pelvic cavity.
However, experiencing reflux symptoms during pregnancy can predispose women to the same symptoms postpartum. It is estimated that about 20% of women continue to experience reflux symptoms even after giving birth.
Fortunately, symptoms have no adverse, long-term effects during pregnancy other than short-term discomfort. Severe complications are rare due to the shorter time frame in which women are affected; damage to the esophagus as a result of reflux takes years.
Lifestyle/Diet Changes
“Step up” management of reflux and heartburn is recommended. With this method, women attempt to reduce symptoms through lifestyle and diet changes first, followed by non-pharmaceutical remedies and/or medications if lifestyle/diet changes do not effectively reduce symptoms.
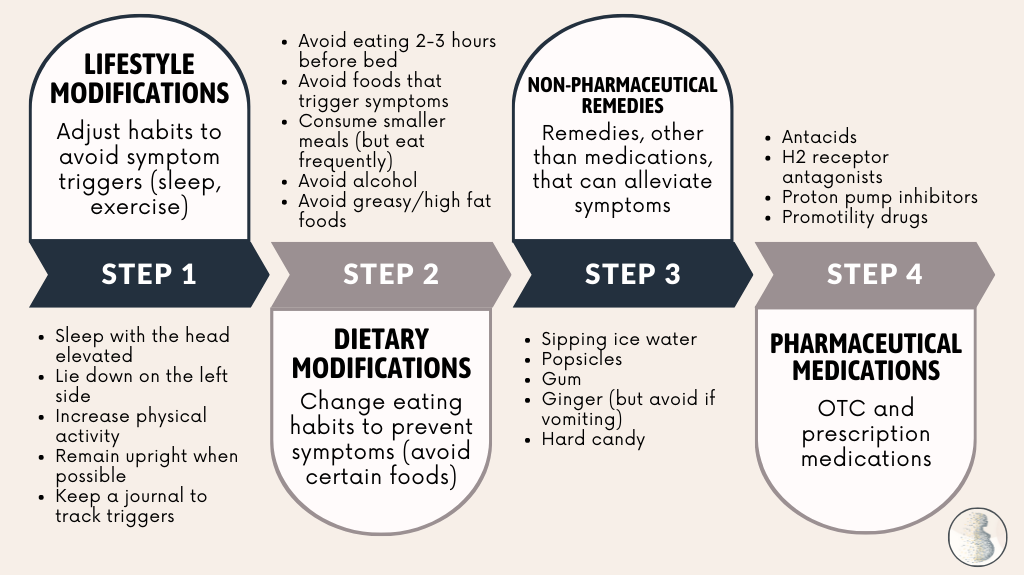
The top lifestyle/diet recommendation includes eating smaller meals more frequently to avoid additional pressure in the abdomen; this may also include eating solids and drinking liquids separately, rather than during the same meal.
Women should also try to avoid eating foods that can exacerbate reflux and heartburn, such as spicy and greasy foods, tomato products, chocolate, coffee, and caffeine (see Action and Resources sections for more information, including a list of reflux-inducing foods).
A study from 2015 found that consumption of green vegetables were found to be protective against heartburn and more frequent consumption proportionally decreased the risk of reflux symptoms.
Reflux symptoms generally worsen when lying down. It's best to wait at least 2 to 3 hours after eating before going to sleep or laying flat, to include lying on the side.
Women should also:
Try sleeping with the head/shoulders elevated on 2 to 3 pillows so gravity can assist in keep reflux down. However, some sources indicate this is not very effective, and that women should actually elevate the bed 6 to 8 inches (15 to 20 cm) by using foam blocks under the top frame of the bed or firm foam (wedge shape) blocks underneath the top part of the mattress.
Consider chewing gum to neutralize stomach acid through the production of more saliva, but this may also cause bloating.
Suck on hard candy to eliminate any bad taste in the mouth as a result of stomach acid.
Sip ice cold water or consume popsicles to eliminate bad taste and “cool” down any burning feeling, albeit temporarily.
Medications
Antacids containing aluminum and calcium are considered safe during pregnancy and are first-line treatments for heartburn and acid reflux when taken in appropriate doses, and according to an HCP’s instructions.
Although concerns regarding aluminum consumption are common in the scientific community, there is no consistent evidence that aluminum exposure due to antacid use is harmful during pregnancy when taken as directed. However, women have other options as well.

Most antacids contain calcium in the form of calcium carbonate and calcium citrate.
Although generally well tolerated, antacids may cause constipation and can interfere with the absorption of some foods and supplements. Women should talk to their HCP with any questions regarding dosage and timing of antacids with other medications.
Magnesium-containing oral antacids should be avoided in the last trimester due to magnesium potentially interfering with contractions. Too much magnesium can also cause nausea, vomiting, and diarrhea. Antacids containing sodium bicarbonate (baking soda) should also by avoided because they may cause a buildup of fluid.
Note: Pregnant women should not use or take heartburn tablets solely to obtain extra calcium; however, pregnant women who do take them for symptom control can use the tablets toward a daily calcium requirement.
Antacids while breastfeeding: Data on the use of antacids while breastfeeding are scarce. However, aluminum, calcium, and magnesium are poorly absorbed orally and are not expected to enter breast milk beyond negligible amounts. (In general, breast milk has lower levels of aluminum than cow’s milk and infant formula.)
Sucralfate (aluminum salt) has been used for decades for the treatment of peptic ulcers and is sometimes used as a first-line therapy for heartburn symptoms during pregnancy. Sucralfate appears to be safe in pregnancy as it is minimally absorbed. It has also not been shown to be harmful in animal studies using doses 50 times more than the standard dose in humans. Its most common side effect is constipation.
Antihistamines are also used to reduce the secretion of gastric acids and are considered safe during pregnancy (more detail). Antihistamines are generally used after lifestyle changes and/or antacids have already been tried. Antihistamines are also commonly used to treat nausea and vomiting of pregnancy.
Note: Ranitidine (Zantac) was an antihistamine that was U.S. Food and Drug Administration (FDA) approved for the treatment of peptic ulcers and reflux/heartburn symptoms.
In October 2019, the drug was identified to contain low levels of N-nitrosodimethylamine (NDMA), a probable carcinogen. FDA had allowed the drug to remain on the market, but it was voluntarily recalled by the manufacturer (USP 150 mg, 100 count Unit Dose Blisters).
However, in April 2020, the FDA advised manufacturers of ranitidine to pull it from the market immediately after determining levels of NDMA in the medication increases over time as well as when stored at higher temperatures, resulting in possible exposure in some individuals over acceptable levels. Ranitidine products are no longer available via existing prescriptions or over-the-counter (OTC) use in the U.S.
Sodium alginate (liquid Gaviscon®): In a study published in 2012, the researchers of a prospective open-label study in a large number of pregnant women showed "that [liquid Gaviscon] is both safe and highly efficacious in the treatment of heartburn and GER symptoms in pregnancy."
Alginate absorption is limited and alginates are not significantly metabolized; therefore, alginates are considered while breastfeeding.
Proton pump inhibitors (PPI), such as omeprazole, inhibit stomach enzymes involved in acid production. Although considered safe during pregnancy, PPIs are generally recommended for pregnant women who have had no success with dietary changes, antacids, or antihistamines. However, PPIs may reduce iron absorption.
Most PPIs are excreted into breast milk hundreds of times lower than doses given to infants who have reflux, and are therefore expected to be safe while breastfeeding.
Action
Women should talk with their HCP if they are concerned about acid reflux, are suffering from NVP that may be caused by reflux, or have heartburn symptoms – before taking any over-the-counter medications. HCPs can also recommend additional lifestyle/diet modifications that could provide further temporary relief.
Women should also consider sharing and submitting their experience below regarding acid reflux and heartburn during pregnancy. This can help other women learn additional perspectives regarding this concern and how to potentially manage their symptoms.
Resources
Problems of the Digestive System (American College of Obstetricians and Gynecologists)
Diet and Gastroesophageal Reflux Disease Infographic (American Society for Gastrointestinal Endoscopy)
Acid Reflux (American College of Gastroenterology)
GERD Diet: Foods That Help with Acid Reflux (Johns Hopkins Medicine)
Diet Changes for GERD (International Foundation for Gastrointestinal Disorders)