Bladder and Pelvic Floor

The bladder and pelvic floor changes that occur during both pregnancy and vaginal delivery can potentially cause urinary problems. Fortunately, most women will completely recover from these symptoms/conditions a few weeks to a few months postpartum.
The bladder and urethra lose muscle tone during pregnancy and weaken; the bladder also holds less urine as pregnancy progresses. The pelvic floor muscles that support these organs also weaken due to hormonal effects and uterine weight, leading to symptoms such as leaking, frequency, trouble voiding, and strong urges to urinate.
Although bladder and pelvic floor complications can occur (i.e. prolapse) these are relatively rare and can also be treated.
It is important to note that pregnancy itself can cause these changes and symptoms, not just vaginal delivery; cesarean section does not completely prevent urinary problems, nor is it recommended for this purpose.
Women should understand changes to the bladder and pelvic floor during pregnancy to better recognize why and when symptoms may occur, and when to have a discussion with their HCP.
Background
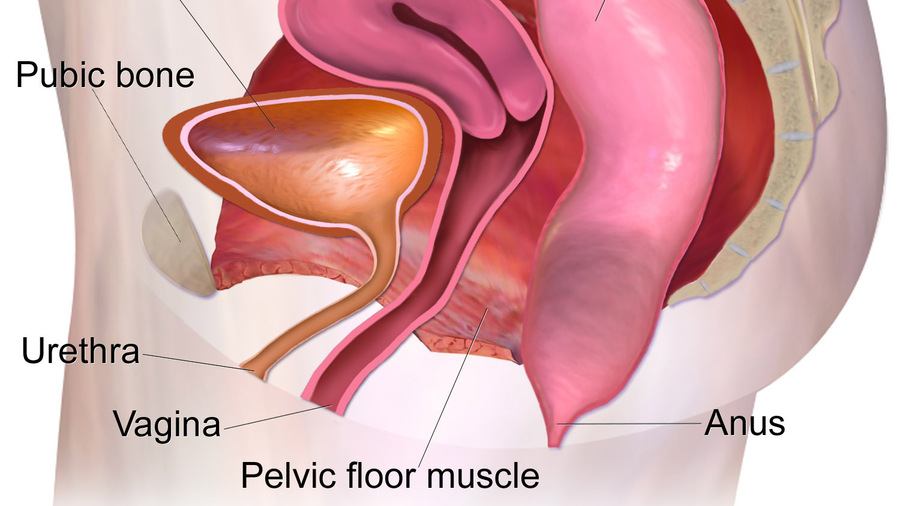
The bladder is located above the pelvic bones and supported by the pelvic muscles. The urethra is a tube that allows urine to flow out of the bladder. Pregnancy causes significant changes to all these structures and these changes are strongly associated with a variety of urinary-related symptoms.

Bladder
Pregnancy (and its related hormones) causes reduced muscle tone in the bladder, ureters, and urethra starting in the third month. As pregnancy progresses, the bladder gradually stretches, loses more muscle tone, changes shape, and gets displaced upward toward the abdomen.
Normally, the bladder muscle relaxes as the bladder fills with urine, while the sphincter muscles help to keep the bladder closed until they are relaxed just prior to purposeful urination. When these muscles lose tone, they weaken.
When a pregnant woman coughs, sneezes, laughs, or moves, intra-abdominal pressure increases, and this pressure is transferred to the bladder. When pressure is too great, the already weakened sphincter gives with only minimal pressure, and leakage results.
The bladder varies in how much urine it can hold during different times in pregnancy:
Normal bladder capacity in the first trimester is approximately 410 milliliters (ml) (average adult bladder holds 400 to 700 ml). Bladder capacity increases in the second trimester to about 460 ml, but dramatically decreases in the third trimester to approximately 272 ml due to engagement of the baby’s head, which leads to increased frequency near term.
After delivery, bladder neck mobility increases, which can lead to leaking (incontinence issues) in the postpartum period. Of note, while vaginal delivery has a more significant impact on bladder neck mobility, pregnancy itself also does (cesarean section does not necessarily protect against these concerns).
Pelvic Floor
The increasing pressure/weight of the growing uterus on pelvic floor muscles weakens them, leading to a peak of urinary symptom severity in the third trimester.
The “u-shaped” opening in the pelvic floor muscles through which the urethra, vagina, and rectum pass has been shown to be significantly larger at 37 weeks of pregnancy and at 6 weeks postpartum compared with earlier during pregnancy.
Women who have had more than one pregnancy are far more likely to experience urinary tract symptoms due to a cumulative loss of pelvic floor muscle strength, as these muscles do not always completely heal between pregnancies.
A second pregnancy can decrease pelvic floor muscle strength at a rate of 22% to 35% beginning at a week 20, potentially lasting until six weeks postpartum.
Since the pelvic muscles support the position of the bladder, as they weaken, the bladder can drop in some women, even to the level of the hymen, which is considered normal during pregnancy and generally resolves after delivery.
However, bulging of the bladder into the vagina is called bladder prolapse, or a cystocele; the urethra and rectum can also drop down.
Although up to one-third of all women are assessed to experience pelvic organ prolapse to some degree, the prevalence of women experiencing this condition due to pregnancy is very difficult to determine.
Some women may be asymptomatic, and diagnosis requires physical examination and possible medical imaging in some cases; further, some women may have symptoms but do not seek treatment.
Delivery
Although pregnancy itself can cause urinary problems during and into postpartum, vaginal delivery can further increase the risks for these symptoms (“increased risk” does not mean the below is always going to occur, and many women will heal with no lasting effects).
Labor and delivery may stretch, strain, or tear the supporting muscles and tissues that hold the uterus, bladder and rectum in their proper place.
Pelvic nerves that control bladder function may be injured during a long or difficult vaginal delivery.
Delivery with forceps can result in injuries to the pelvic floor and anal sphincter muscles, as they allow more room for delivery.
As the head comes out, the force of pushing may tear the ligaments that anchor the pelvic muscles to the pelvic bones; most women are urged to push slowly at this stage to prevent injury.

Delivery can also (uncommonly) cause prolapse of various pelvic organs (uterus, urethra, bladder, rectum).
Cesarean section can avoid stretching and tearing of the muscles and nerves that may occur due to vaginal delivery, but does not prevent bladder/pelvic muscle injury that occurs as a result of pregnancy itself. As also stated above, cesarean section also carries its own risks to the bladder.
Postpartum
It is possible to experience temporary nerve issues after delivery, which decreases the sensation of needing to urinate; further, temporary swelling immediately after delivery can also impact the ability to urinate.
In most cases, damage created by vaginal delivery repairs itself, as tissues, nerves, and muscles heal; even severe symptoms can dramatically improve within the first six months.
However, the bladder continues to lose muscle tone in the early postpartum period, and damaged muscles and ligaments may not always heal completely in some cases. Leaking can become a problem as the muscles further weaken through age or additional pregnancies. Bladder neck mobility does improve (decrease) up to six months postpartum, but not all women will return to pre-pregnancy mobility.
Even still, only about 5% of women still have stress incontinence a year after delivery.
Action
If a woman is very concerned or even fearful about protecting the urinary system from vaginal delivery, she should have a conversation with her HCP. HCPs can recommend certain exercises and even physical therapists who can help women strengthen their pelvic floor.
While some women may want an elective cesarean section to avoid possible urinary complications, cesarean section is not completely protective of urinary/bladder injury.
Women should read Urinary Problems for more information specific to leakage, trouble voiding, and frequency (to include Kegel exercises).
Women should also read the personal experiences of other women who have experienced urinary system changes and symptoms during pregnancy.
Resources
Pregnancy and Bladder Control (Cleveland Clinic)
Caring for your Bladder During and after Delivery (University of Michigan Health System)
The Pelvic Floor Muscles - a Guide for Women (Pelvic Obstetric and Gynaecological Physiotherapy)