Kidneys

Kidneys work a lot harder during pregnancy. They are responsible for a significant increase in both urine production and the elimination of waste, and maintain the critical balance between sodium and fluid.
While this process is not well understood during pregnancy, it is clear that keeping kidneys healthy can prevent numerous potential complications and ease urinary symptoms.
Women should tell their HCP about any urinary symptoms they are experiencing, to include frequency, trouble voiding, leaking, and painful urination, as well as pelvic and lower back pain. These symptoms could all indicate possible infection or complications that need to be evaluated.
Women should remain properly hydrated, exercise regularly, avoid excess sodium (although restriction is not necessary) and talk to their HCP if they have any questions or concerns.
Background
The kidney is responsible for regulating water, electrolyte balance, and blood pressure, as well as removing waste from the body. Pregnancy affects all these aspects of the kidney, as well as its size, structure, and function.
Glomerular Filtration Rate
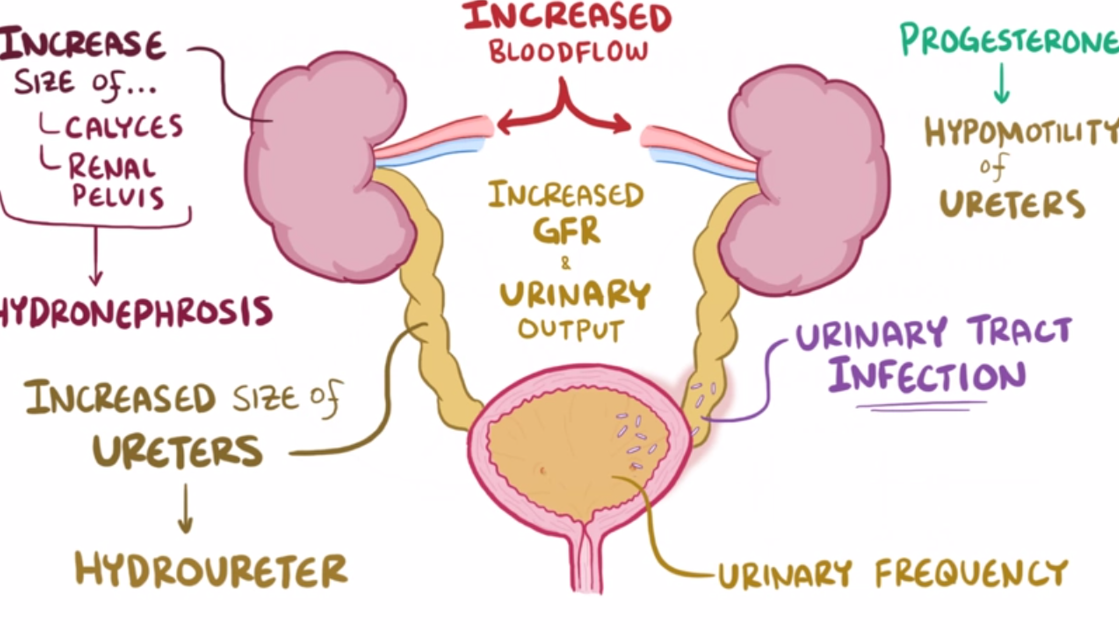
One of the earliest kidney changes during pregnancy is the rise in glomerular filtration rate (GFR); the initial process in urine production.
GFR rises as much as 25% by the second week after fertilization and 50% by the beginning of the 2nd trimester.
The glomerulus is the filtering unit of the kidney. On average, there are one million nephrons in each adult kidney, and each nephron contains a glomerulus. This system filters approximately 200 liters of fluid a day in non-pregnant individuals. Although the approximate number of liters filtered during pregnancy has not been studied, it is theorized to be almost 250 to 300 liters, based on the increased filtration rate.
The fast, increasing rise of human chorionic gonadotrophin (HCG) causes more blood to flow to the kidneys, which leads the kidneys to eliminate waste quicker than prior to pregnancy. This also leads to increased urinary frequency so early in pregnancy, well before the uterus puts pressure on the bladder.

This increased frequency and GFR leads to greater thirst. However, increased fluid intake (i.e. drinking water) reduces sodium levels in the blood, so the body begins to retain sodium – leading to a retention of fluid, and therefore swelling results. It is estimated the body retains an extra 4 to 8 liters worth of fluid during pregnancy. All this fluid is filtered by the kidneys.
Due to fluid retention, the length of the kidneys can increase by as much as 1.5 centimeters, and volume can increase by as much as 30%. The kidneys will decrease in size back to normal around four to six months postpartum. These changes may be permanent, however, in approximately 11% of women.
Due to faster clearance in the kidney, it is theorized that normal doses of certain antibiotics and other medications may be ineffective; pregnant women may need more medication in a specific period of time versus non-pregnant women. However, there is very little research to confirm this theory, and very little data overall regarding medications and pregnancy.
Swelling of the kidneys can occur in 43% to 100% of pregnant women and is more prevalent as pregnancy progresses (not dangerous):
Hydronephrosis, swelling of one or both kidneys due to a blockage or obstruction of the kidneys’ urine collection system, occurs in most pregnant women beginning around 22 weeks of pregnancy. This is considered normal and asymptomatic – unless an infection develops.
This blockage can trap 200 to 300 milliliters of urine in the system when it should be empty. This is assessed to be a leading contributing factor to the high prevalence of Urinary Tract Infections during pregnancy.
Potential Problems
Impaired renal (kidney) function during pregnancy is considered relatively common and can increase the risk of complications.
Dehydration can negatively affect the kidneys; they function more efficiently in the presence of plenty of water.
Dark urine is often indicated as a sign of dehydration. When there is not enough water in the body, the kidneys produce a more concentrated urine, which requires more energy and causes greater wear on the kidney’s tissues.
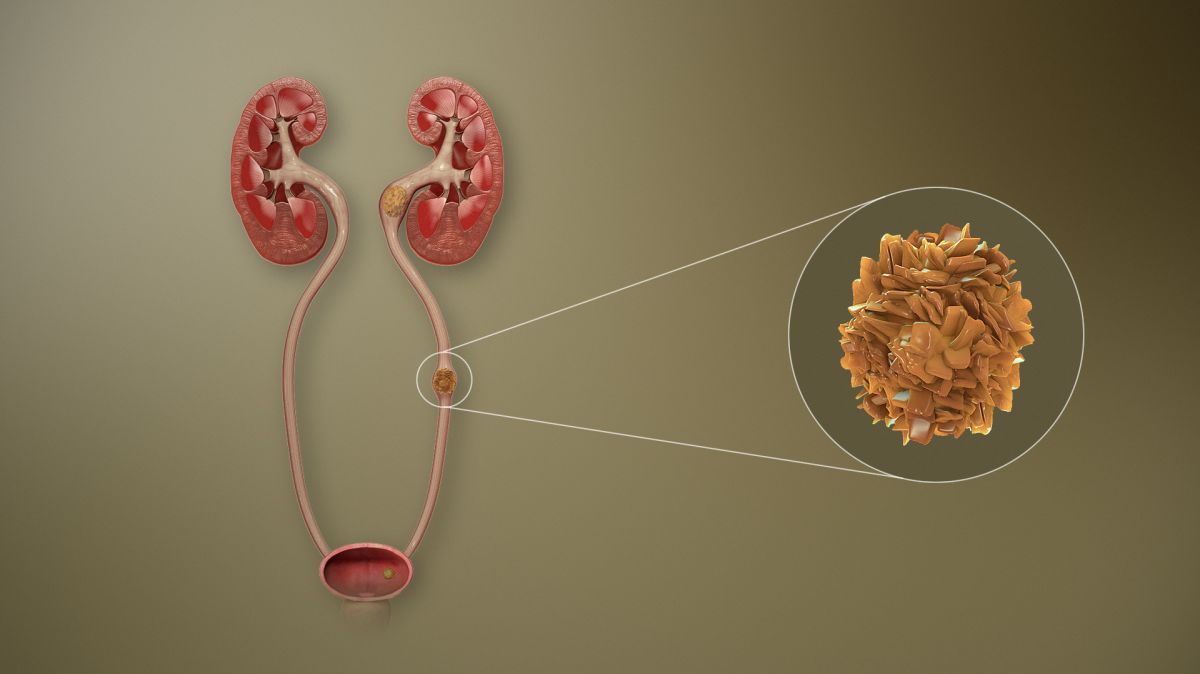
Prolonged or repeated bouts of dehydration (such as with nausea and vomiting of pregnancy) can cause urinary tract infections, kidney stones, and even kidney failure.
A study published in April 2021 indicated that pregnancy increases the risk of a first-time symptomatic kidney stone that peaks close to delivery and then improves by 1 year after delivery. Risk appears to be highest during the first three months postpartum.
Kidney stones are reportedly detected in 1 in 90 to 1 in 3,800 pregnancies. Although 70% to 80% of stones will pass on their own, hospitalization may be required due to pain.
High blood pressure, one of the signs of preeclampsia, can affect kidney function. Severe preeclampsia accounts for about 40% of acute kidney injury during pregnancy. HELLP Syndrome and Acute Fatty Liver of Pregnancy also affect kidney function. All these conditions likely share some of the same underlying causes.
Due to the amount of work and increased function of the kidneys, pre-existing kidney disease can be accelerated during pregnancy, resulting in a worsening of their function. It is important women understand their medical history and tell their HCP if they have had or currently have any issues related to their kidneys. Moderate to severe kidney disease can also result in an increased risk for preterm delivery and preeclampsia.
For those who have chronic kidney disease (CKD), pregnancy outcome is related to impaired glomerular filtration rate and the degree of proteinuria (see below section).
A study published in October 2021 determined that for those with CKD, proteinuria and serum creatinine level should be examined before pregnancy and regularly monitored during pregnancy. Higher creatinine levels and higher proteinuria may lead to preterm birth and lower birth weight of the newborn.
Proteinuria
Proteinuria assessment is important for the determination of kidney health during pregnancy. Proteinuria is characterized by an abnormal amount of protein in the urine; with increasing proteinuria, there is an increased risk of pregnancy complications. Healthy kidneys do not allow an excess amount of protein to pass into the urine.
The screening tool used to assess the level of protein in the urine is known as a dipstick test and is done in an HCP’s office by dipping a test strip into a cup of urine.
The amount of protein in the urine increases during normal pregnancy, from less than 150 milligrams (mg)/day in non-pregnant individuals to up to 300 mg/day in pregnancy.
Note: The diagnostic criteria for preeclampsia has changed as researchers learn more about the condition. Proteinuria used to be a mandatory finding for the diagnosis of preeclampsia but is considered no longer necessary (read more).
The dipstick test is still important to perform at routine prenatal appointments as the presence of increased protein in the urine indicates inflammation, and is also associated with preterm labor, premature rupture of membrane, and intrauterine growth restriction.
Postpartum
After delivery, the kidneys continue to work hard to eliminate extra fluid. Fluid levels slowly return to normal about eight weeks postpartum, which mainly occurs through frequent urination and sweating, especially the first week after delivery.

Action
Women should tell their HCP about any urinary symptoms they are experiencing, to include frequency, trouble voiding, leaking, and painful urination, as well as pelvic and lower back pain. These symptoms could all indicate possible infection or complications that need to be evaluated.
Note: Pre-existing kidney disease can be accelerated during pregnancy, resulting in a worsening of their function. It is important women understand their medical history and tell their HCP if they have had, or currently have, any issues related to their kidneys.
To maintain proper kidney health, women should exercise regularly and remain hydrated.
However, while staying properly hydrated can help improve kidney function, it is also important women do not become over hydrated, which depletes sodium and other electrolytes within the body and can lead to its own set of complications.
Unfortunately, the exact amount of water or other fluids pregnant women should consume each day is not known, and likely varies considerably from woman to woman. In addition, in healthy pregnancies, sodium restriction is likely not necessary.
Pregnant women should ask their HCP any questions they have regarding fluid intake, exercise, swelling, urinary symptoms, and kidney health.
Resources
Urinary Tract System (National Urinary Foundation, American Urological Association)