Tearing (and Episiotomy)

Research indicates that education about episiotomies is important to women and helps them feel more comfortable with the birthing process. More specifically, written information on these topics was shown to increase acceptance and reduce anxiety levels (Alexander et al. 2019).
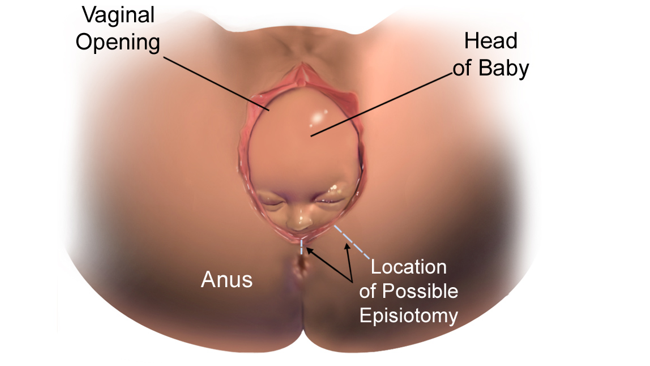
Crowning – the term used for when the widest part of the baby’s head arrives at the vaginal opening – can cause some women to tear through various tissues in the vaginal, perineal, anal, and/or rectal areas (but not always).
Most women tear to some degree with their first vaginal delivery, but only a small percentage experience more severe tearing.
An episiotomy – a purposeful incision made by a health care provider about halfway into the perineum – was used routinely until the early 2000s, as it was believed the procedure would avoid the possibility that a woman would end up with a more severe tear unless a “controlled” incision was made.
Today, however, episiotomies are only performed under strict circumstances as almost all evidence completed since the 1980s indicates that episiotomies have almost no benefit unless the baby needs to come out as soon as possible.
Further, episiotomies do not prevent further tearing, they do not improve postpartum healing (i.e. a straight vs. jagged tear) and they are not always needed for assisted delivery (vacuum/forceps).
Pregnant women should ask their HCP about the HCP's use of episiotomies, how often they perform them, and when the HCP thinks they are necessary during delivery.
Background
An episiotomy is a purposeful cut made in the perineum – the area between the vagina and anus during labor and delivery. An episiotomy used to be the most performed procedure in obstetrics until research showed – after almost two decades of its routine use – that an episiotomy served no benefit during delivery unless a baby needed to be born as soon as possible.
A normal vaginal delivery can cause tears to the vagina, the surrounding tissue, and sometimes to the rectum. These tears can be repaired, but for some women, healing can be prolonged, and some women may have pain into the extended postpartum period.
This image contains triggers for: Real Delivery
You control trigger warnings in your account settings.
Episiotomies became popular in the 1980s when it was theorized that a purposeful, clean cut with scissors or a scalpel into the perineum could prevent women from having a much deeper, jagged, uncontrolled tear (i.e. a “smaller” cut was therefore beneficial because it would prevent a much “larger one”). It was thought it could also speed up delivery and prevent other tearing-related postpartum complications.
A popular pregnancy book published in 1980 indicated that episiotomies were increasingly performed in the United States (U.S.) and in some estimates, 100% of mothers received an episiotomy.
The increased use of this procedure was also a part of the establishment of the active management of labor. Active management by an HCP includes taking purposeful steps to speed up labor, even if there is technically no medical reason to do so (some women may choose active management).
Today, about 11% to 14% of women in the U.S. receive an episiotomy during vaginal delivery.
Tearing – General
Crowning is the term used to describe when the widest part of the baby’s head remains at the vaginal opening. Because the skin in the vaginal and perineal areas need to stretch to their full capability at this time, women may feel a burning (“ring of fire”), stinging, or a numbness. Although these tissues are designed to stretch to a significant degree, some women will still tear.
An HCP may help the woman avoid tearing during crowning by asking the woman to take quick short breaths and to avoid forcefully pushing the rest of the baby out. If the baby’s head is slowly guided out, this could cause a more gradual stretch and possibly prevent severe tearing.
Tears are described in degrees:
First degree: skin layer only
Second degree (most common): midway between the vagina and the anus (halfway through perineum); involves skin and muscle
Third degree: involves skin, muscle, and rectal sphincter
Fourth degree (least common): extending through the rectum; involves skin, muscles, rectal sphincter, and anal wall (the anus is the opening of the bowel, the rectum is inside the body, above the anus)
Occasionally, a tear may occur at the top of the vagina, known as a periurethral laceration, that may require a few sutures (stitches).
Episiotomy Recommendations
Since the early 2000s, restrictive (or selective – “case by case”) episiotomy has been recommended over routine (automatic) use.
Current research indicates that episiotomies do not provide any benefit in a normal delivery to either the mother or the baby – unless a baby is in distress and needs to be born as soon as possible.
However, some organizations do still believe that a controlled “cut” may be better than an uncontrolled tear.
Most studies evaluated vaginal and perineal injuries in mothers who received an episiotomy and those in a “selective” group (only when it was felt to be necessary). It was consistently found that women in the selective groups recovered faster, had less trauma, had significantly less pain, and fewer overall complications than the group that received a routine episiotomy (i.e. no matter what).
This research indicated that despite prior thought that episiotomy would result in a “lesser” tear than what women would "naturally" receive, the opposite appeared to be true – women were receiving episiotomies when they were unlikely to tear at all, or to a very minimal degree. Therefore, women were potentially subjected to unnecessary pain and trauma to the vaginal/perineal area. Further, episiotomies were strongly associated with the same risks they were originally used to prevent.
Additionally, episiotomy has also been associated with an increased risk of repeated episiotomy and spontaneous perineal tears in a subsequent delivery.
Based on the above, current recommendations advise the selective or restrictive use of episiotomy; it should be avoided if at all possible, but may be required in very specific circumstances, mostly determined by the HCP’s clinical judgment.
Episiotomy is now performed on an individualized basis. If the baby is showing signs of distress, then episiotomy – in this case – may speed up labor and lead to delivery faster. This benefit would outweigh all known potential risks associated with the procedure.

Some recommendations also include the possibility of an episiotomy in the case of assisted delivery (vacuum/forceps) (although selective/restrictive use may still be reasonable).
There is some evidence that in the case of forceps or vacuum, the use of a mediolateral (see below) episiotomy is associated with a five-to-tenfold reduction in the rate of obstetric anal sphincter injuries, as significant tearing is much more likely with assisted delivery.
Episiotomy Procedure
The decision about whether to have an episiotomy cannot be made until delivery and fetal heart rate/movements are monitored. An HCP will advise the woman if an episiotomy is required to necessitate delivery.
Prior to the incision, a local anesthetic is applied, or more medication is provided through an epidural if one was already placed.
The two most common types of episiotomy are:
Midline: a cut from the vagina directly towards the anus.
Mediolateral: a cut from the vagina at an angle off to one side of the anus (more common)
The HCP will use scissors or a scalpel to make a 2 to 4 centimeter incision.
Episiotomies are measured in the same degrees as tearing (see above).
The incision is repaired after the placenta has been delivered, and usually while the woman is holding her baby. Episiotomies are repaired with sutures that will eventually dissolve on their own. Additional anesthetic may be given for repair as well.
Some possible complications of an episiotomy may include (similar to complications associated with tearing in general):
Bleeding
Tearing into the rectal tissues and anal sphincter muscle
Swelling
Infection
Hematoma
Pain during sex
Scar tissue formation
Painful urination
Action (and Healing)
Pregnant women should ask their HCP about the HCP's use of episiotomies, how often they perform them, and when the HCP thinks they are necessary during delivery.
However, regardless of whether an episiotomy occurred, vaginal injury is common after vaginal delivery and women should ask their health care provider what they should expect (pain, recovery time) in those first few weeks postpartum.
Women's recovery can vary widely; some women experience minimal pain while others have more severe pain that could last more than a week or two (but rarely "chronic"). A study published in June 2021 indicated that based on women's different experiences, postpartum pain management should be very individualized.
Women have numerous options for managing pain and avoiding longer-term complications by:
Using a “peri bottle” while in the bathroom: this type of bottle can be filled with warm water that is then sprayed over the perineum while emptying the bladder – which can ease any pain. The hospital/birthing center will likely provide one in the postpartum room; women can also buy their own (they come in different designs) at various drug stores.
Applying an ice pack: labor and delivery nurses can make ice packs from newborn diapers that may be more comfortable to sit on then a standard ice pack; they also have a better "direct" design for the area. Learn how to make one here (1:32 seconds; video is straight to the point).
Using a sitz bath: a sitz bath is a small, shallow, plastic basin filled with cool or warm water; the "bath" has just several inches of water that is then used to submerge the perineal area, possibly up to the hips. The basin fits on top of a toilet seat and women can slowly lower their hips into the water. Hospitals and birthing centers provide one, but women can also buy their own.
Using witch hazel pads: witch hazel is an astringent with a cooling effect; pads soaked in witch hazel can be placed in a woman's postpartum clothing or on top of a diaper ice pack to help reduce swelling and inflammation; witch hazel is also available without prescription and is usually provided to postpartum women at their facility.
Sitting on a pillow: women should sit gently on pillows to ease pain; some pillows are specifically designed for this purpose; women should also move and get up slowly off couches and chairs to avoid further injury.
Asking their HCP about numbing sprays or creams: most hospitals/birthing centers also provide at least one type of these medications to postpartum women; they are also available over the counter without a prescription, but women should ask their HCP prior to purchasing a different type.
Resources
Watch how an episiotomy is performed here (start at 0:20 second mark) (uses a model, not a real delivery; *needle trigger)
Prevention and Management of Obstetric Lacerations at Vaginal Delivery (American College of Obstetricians and Gynecologists)
First-and Second-Degree Tears (Royal College of Obstetricians and Gynaecologists)
Third-and Fourth-Degree Tears (Royal College of Obstetricians and Gynaecologists)
Episiotomy (Royal College of Obstetricians and Gynaecologists)
Slide show: Vaginal tears in childbirth (NCH Healthcare System)