Migraine

Migraines are considered a distinct entity from other types of headaches; they can range in severity from mild to utterly debilitating, lasting several hours in duration to two weeks or longer.
Recent research (2020-2022) is starting to highlight the higher risk of adverse pregnancy outcomes in women who suffer migraines during pregnancy (read "Complications" section). If you suffer from migraines and are trying to conceive or are currently pregnant, talk to your health care provider (HCP) who can help you determine the best management plan during pregnancy.
Fortunately, almost three-quarters of women who suffered from migraines prior to pregnancy will have significant relief, if not complete relief, during pregnancy. This is theorized to occur due to hormone stabilization after the first trimester, whereas hormone fluctuations occur much more often and rapidly during the menstrual cycle.
It is possible that some women may experience their first migraine during pregnancy, which needs to be assessed by an HCP to confirm the likelihood of a migraine rather than a different type of headache, as well as rule out other possible causes (high blood pressure, preeclampsia).
Women do not have to suffer through headaches during pregnancy. By talking with their HCP, they can engage in risks and benefits discussions regarding safe management options for migraines – and other headaches – during pregnancy.
Background
Migraine headaches are a relatively common type of headache in pregnancy (although most women experience significant relief). These painful, throbbing headaches are usually felt on one side of the head and result from expansion of the blood vessels in the brain; they also appear to be influenced by genetics and the environment.
Migraine pain ranges from mild to severe to utterly debilitating. They can last for hours to days, and some women may experience migraines for two weeks of every month or longer.
Migraine is a predominantly female disorder that can be greatly influenced by hormones and their fluctuations (primarily estrogen). During pregnancy, estrogen may reach one hundred times a woman’s normal level.
Despite migraine being is the most common neurological cause of disability in the world, it is still not well understood – especially regarding treatment.
Symptoms
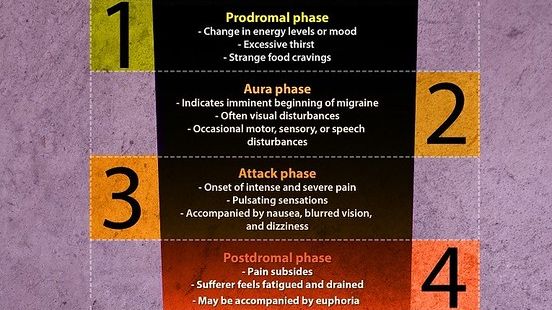
Migraine typically presents with throbbing and pulsating pain on one side of the head that is exacerbated by physical activity (due to the vascular nature of the condition).
Migraine is classified in two ways: migraine without aura and migraine with aura. An aura consists of neurological anomalies that can occur before, during, or after a migraine that can include flashes of light and/or limb numbness or tingling. Aura is thought to occur due to decreased blood flow to the brain.
Migraine can also cause nausea and vomiting, even from just moving the head, as well as sensitivity to light and sound.
Pregnancy
About 50% to 75% of women experience a marked improvement in their migraines during pregnancy with a significant reduction in frequency and intensity of their attacks. Some of these women will experience complete relief, especially if they suffered from menstrual migraines.
Since some migraines (and most headaches) occur, or get worse, due to blood vessel expansion in the head, theoretically, migraines should always get worse during pregnancy due to the significant increase in blood volume.
However, some studies have shown that this increase in blood volume does not appear to affect the brain as it does other parts of the body and may be a key factor in most headache improvement in pregnancy (read Brain).
Further, migraine headaches are known to be influenced by cyclical changes in reproductive hormones; it is thought the absence of hormonal fluctuation during pregnancy is responsible for improvement. After delivery, most women quickly return to their pre-pregnancy migraine pattern.
In contrast, it is estimated that approximately 8% of women experience increased frequency or intensity of their migraines during pregnancy.
In the small number of women whose migraines worsen, these women tend to also experience aura; it is possible women who suffer with migraine without aura better tolerate the hormonal changes of pregnancy. It is also assessed that migraines that persist into the second trimester are less likely to improve.
New-onset migraine headache can occur in up to 16% of pregnant women and usually presents in the first trimester. It is recommended that when migraine first occurs during pregnancy, HCPs should consider an MRI (no radiation) to be cautious and rule out other possible causes.
If women experience severe pain on both sides of the head, and have high blood pressure, preeclampsia and eclampsia also need to be considered. It estimated that up to one-third of women who present with a new onset of headache pattern during pregnancy have preeclampsia.

Complications
In general, migraine itself does not cause complications during pregnancy unless the pain is debilitating for the mother. However, migraine could increase the risk of complications, or it could be an indicator of other problems, such as high blood pressure and preeclampsia (mentioned above).
A study published in May 2022 in the journal of the American Academy of Neurology found that migraine is an under-recognized risk factor for adverse pregnancy outcomes, especially high blood pressure disorders and preterm delivery. The authors indicated that "patients who report migraine history may warrant closer monitoring during pregnancy."
A study presented at the American Academy of Neurology 74th Annual Meeting in February 2022 found that pre-pregnancy migraine was associated with higher risks of preterm delivery, gestational hypertension, and preeclampsia. Migraine with aura was associated with a somewhat higher risk of preeclampsia.
A study presented at the 7th Congress of the European Academy of Neurology in June 2021 determined that pregnant women with migraine were at increased risk of having obstetric and medical complications compared with unaffected women, and therefore should be included in a high-risk pregnancy protocol of care throughout pregnancy.
Additional studies have found that patients with migraine may have an elevated risk for depression, anxiety, stress, preeclampsia, and /or stroke during pregnancy, which could remain during the postpartum period. Migraine during the first trimester is also associated with a higher risk of nausea and vomiting, as well as hyperemesis gravidarum.
Management
Migraine management – which includes treatment and prevention – ranges greatly, depending on severity and frequency of attacks.
Treatment can include non-steroidal anti-inflammatory drugs (NSAIDs) and combination analgesics (acetaminophen and others) — to migraine-specific drugs, including ergotamine preparations and triptans as well as antiemetics (anti-nausea).
Women should have a risks and benefits discussion with their HCP regarding migraine medications during pregnancy and should aim to use the lowest dose of any medication for the shortest amount of time necessary.
Acetaminophen is a safe treatment and is often the first-line recommended treatment for any pain during pregnancy, but it may not be very effective against painful migraine. Acetaminophen, together with codeine, is commonly prescribed for migraines during pregnancy.
NSAIDs (ibuprofen, naproxen) are recommended as a second choice if used sparingly and for a short amount of time; they should also be avoided during the last trimester due to bleeding concerns.
Triptans were the first drugs specifically developed for migraines and tend to be very effective; however, there can cause significant adverse side effects and data during pregnancy is very limited, albeit reassuring. It is recommended that all other medications with better and more complete safety profiles be tried prior to triptans during pregnancy; some researchers have recommended complete avoidance of triptans until more research is completed.
Action
Women should talk to their HCPs about any headaches or migraines they experience during pregnancy.
As mentioned above, women should seek immediate/emergent medical care if they experience a severe, pounding headache either alone or accompanied by dizziness, blurred vision, flashing lights, nausea and vomiting, or swelling the hands, face, legs, or feet.
Although migraines can be difficult to prevent, the best lifestyle recommendations for the prevention and management of headaches (in general) appear to be: routine physical activity, appropriate hydration, regular eating and sleeping habits, reduction of stress, and the avoidance of known headache triggers.
Women may also find cool rags, sleep masks, dark rooms, and noise cancelling headphones helpful.

Women should also consider sharing and submitting their experience below regarding migraines during pregnancy. This can help other women learn additional perspectives regarding this concern, how to potentially manage symptoms, and how to talk to their HCP.
Partners/Support
Partners/Support can help pregnant women keep track of their headache pattern. This information is very useful for HCPs, and it can be harder for women to do this while they experiencing symptoms.
Further, a woman with a severe headache may not be able to fully communicate, and partners may be the first, in some cases, to recognize the woman needs medical attention.
Although most migraines will go away on their own, as preeclampsia becomes more common, recognizing a headache that may indicate possible preeclampsia or eclampsia can prevent delay in diagnosis as well as serious complications.
Partners should also keep in mind that migraines are not as easily treated as primary headaches. In most cases, the only treatment is time. In these cases, partners/support should do everything they can to ease any burden of chores, household duties, childcare, or other responsibilities so women can focus on getting through their attack.
Resources
Migraine and Other Headache Disorders (American College of Obstetricians and Gynecologists)
Slideshow: Headaches in Pregnancy: Before, During and After (start at slide 7) (Robert Kaniecki, MD, Director, University of Pittsburgh Medical Center Headache Center)