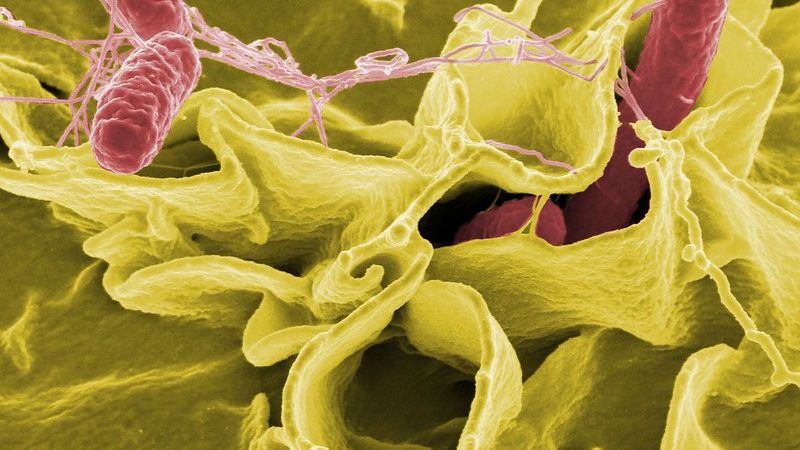
Salmonella

*Outbreak update: As of October 29, 2021, FDA and CDC are investigating several multi-state salmonella outbreaks. Learn more below.
Salmonella infection is a foodborne illness most often contracted through contaminated food such as raw eggs or contact with raw or live poultry (including backyard chickens).
Pregnant women are not generally more susceptible to contracting salmonella, but may experience more severe illness than non-pregnant individuals who contract the infection.
Salmonella mostly causes gastrointestinal symptoms such as diarrhea, nausea and vomiting, as well as fever – with no effect to the fetus.
However, other systemic, more widespread infections can occur during pregnancy; salmonella infection has been documented to cross the placenta and infect the fetus, causing newborn infection.
Fortunately, almost all cases of salmonella can be prevented through proper hygienic practices, adequate cooking of eggs and poultry, and the avoidance of raw food items.
Any pregnant woman suffering from severe gastrointestinal symptoms, or believes she may have contracted salmonella, should call her health care provider (HCP) immediately, or seek emergency care if symptoms are severe.
Background
Salmonellosis is an infection caused by Salmonella bacteria; it is a kind of food poisoning caused by eating contaminated or improperly cooked food. Salmonella affects about 1 to 2 million Americans every year, including 26,500 hospitalizations, and 420 deaths.
In the Europe Union (EU), salmonella affects between 16 and 11,800 per 100,000 people. This dramatically wide range is due to salmonella infection being underreported; most individuals will suffer gastrointestinal illness and recover without seeing an HCP. It is estimated that only 1 of every 57 cases of salmonella infection is reported in the EU.
Causes/Sources
Salmonella bacteria are ubiquitous in the environment and live in the digestive tracts of humans and animals, especially backyard chickens and other farm animals, as well as reptiles and in fish tanks.
Salmonella survives on meat and other animal products that are not thoroughly cooked, which is the main transmission to humans.
Salmonella infections are on an uptick, as raw and unprocessed foods and the increasing trend of backyard chickens, turtles, and hedgehogs as pets (which all carry salmonella) have become more popular.
Contamination can occur through eating and/or touching (without washing hands):
Raw or undercooked poultry, meat or fish
Raw or undercooked eggs (or raw dough/batter)
Unpasteurized milk, milk products and juice (also increase the risk of listeria infection)
Foods that come in contact with animal feces in the soil or water
Cross contamination between raw and cooked foods (read Food Safety)
Unwashed fruits and vegetables (only water is needed; any type of soap is not recommended)

Contamination of eggs and eggshells is a major public health concern. Between 1985 and 2002, contamination of eggs was identified as the source of 53% of all cases of salmonella reported to the U.S. Centers for Disease Control and Prevention (CDC).
Eggs become contaminated with salmonella during the formation of the egg in the reproductive tract of a hen. Indirect contamination occurs after an egg has been laid and salmonella contaminating the outside of the egg penetrates to the inside; salmonella on the shell can also contaminate the egg yolk and white when an individual cracks the egg.
Numerous studies have determined that free range housing eggs have a less incidence of salmonella contamination compared to caged housing, but these eggs are not completely free of infection. However, at least one study found the reverse, likely due to longer interaction in free range housing between the hen and the egg (eggs are removed much faster in caged housing).
Cross contamination and unclean work surfaces in the home are also common sites of infection. One study demonstrated that utensils used to mix raw eggs were sometimes positive even after being washed.
Further, raw batter that was mixed with eggs using a hand whisk or hand-held mixer caused salmonella to spread almost 40 centimeters away from the mixing bowl. Salmonella was noted to survive in raw batter on a surface for at least 24 hours.
Signs and Symptoms
The incubation period is variable but is typically between 6 and 72 hours; some cases can present up to 1 week later; symptoms generally last 2 to 7 days.
The severity of the infection and whether it becomes a systemic (body-wide) infection depends on the resistance of the individual and the virulence of the salmonella strain.
There are technically three clinical forms of salmonellosis:
Gastroenteritis (most common; stays within GI tract; nausea, vomiting, diarrhea, fever)
Septicemia (spreads to blood stream)
Typhoid fever (rare; most severe form, requires immediate antibiotic treatment)
Pregnancy
Pregnant women are not assessed to be more susceptible to salmonella than the general population, with an incidence of 0.2% positive rectal cultures at the time of delivery.
Most salmonella infections during pregnancy do not affect the fetus and outcomes are similar to non-pregnant individuals; however, in severe, systemic cases, salmonella infection during pregnancy can result in the spread of the infection to the fetus. Salmonella bacteria has been identified in amniotic fluid and documented cases of an infected newborn have been reported.
Consequences of infection during pregnancy can cause pregnancy loss, preterm labor, and stillbirth. However, early diagnosis and treatment is associated with a good pregnancy outcome. It is recommended that any pregnant woman with a diarrheal illness should have a stool culture evaluated for salmonella infection.
Management
Salmonella is diagnosed in a laboratory setting with the examination of a stool (fecal) sample.
When salmonella infection remains in the GI tract, management techniques include fluid replacement (avoidance of dehydration), electrolytes if necessary, and controlling pain.
Antibiotics are not recommended in these cases and can prolong recovery. Dehydration and electrolyte imbalance can be more serious during pregnancy, therefore, it is recommended any pregnant woman experiencing diarrhea call their HCP, and if severe, visit an emergency room (see Diarrhea).
For more invasive/severe infections, antibiotic treatment may be necessary. However, there is no consistent standard for antibiotic choice regarding salmonella infection and different regimens are often recommended, with amoxicillin, azithromycin, or cephalosporin recommended most often. Treatment depends on the strain and spread of infection.
Recent Outbreaks
As of October 29, 2021, CDC and FDA are both investigating a large salmonella outbreak linked to onions. All recalled onions were supplied by ProSource Produce LLC and Keeler Family Farms and imported from the State of Chihuahua, Mexico, between July 1, 2021, and August 31, 2021. Do not eat or serve these onions. If you can’t tell where they are from, throw them away. There are currently 808 illnesses and 157 hospitalizations in 37 states linked to this outbreak. Learn more here.
As of October 28, 2021, CDC is investigating a multi-state outbreak of salmonella related to Citterio brand Premium Italian-Style Salame Sticks. They were sold at Trader Joe’s and Wegmans and may be sold at other grocery stores. Do not purchase or eat this product. There are currently 21 illnesses and 6 hospitalizations in 8 states linked to this outbreak. Learn more here.
As of October 8, 2021 (and current through November 7) CDC is investigating a multi-state salmonella outbreak linked to Northeast Seafood Products distributed primarily in Colorado. There are currently 102 illnesses and 19 hospitalizations in 14 states linked to this outbreak:
Seafood types include Haddock, Monkfish, Bone-in Trout, Grouper, Red Snapper, Red Rock Cod, Ocean Perch, Pacific Cod, Halibut, Coho Salmon, Atlantic Salmon Portions, Lane Snapper, Tilapia, All Natural Salmon Fillet, Pacific Sole, and Farm Raised Striped Bass
Sold at seafood counters in Albertsons, Safeway, and Sprouts grocery stores in Colorado
Products were distributed fresh but may have been frozen later by consumers and businesses
CDC has more information on this outbreak here.
ONGOING: As of August 31, 2021 (ongoing as of October 17, 2021), the CDC was monitoring a salmonella outbreak linked to backyard poultry (including chicks and ducklings). There are currently 863 illnesses, 209 hospitalizations, and 2 deaths linked to this outbreak.
According to the CDC, you can get sick from touching backyard poultry or anything in their environment and then touching your mouth or food, and swallowing Salmonella germs.
CDC has more information on this outbreak here.
Action
The shell (of a clean, unbroken egg), the egg yolk, egg white, and the packaging containing the eggs all have the potential to be infected. Avoiding the consumption of raw eggs, and washing hands after cracking eggs, touching the package, or even just the shell, can completely eliminate risk – no matter how slight – and only takes 20 seconds.

Certain guidelines should be followed when handling, storing, and eating eggs or foods than contain eggs:
In general, pregnant women should avoid consuming raw and undercooked eggs, to include homemade foods that often contain raw eggs such as mayonnaise and salad dressings, custards and ice creams, and raw cookie dough and cake batter unless pasteurized eggs have been used. (Note: Raw flour has been increasingly linked to E. coli infections in the United States).
Pasteurized eggs can be purchased (including in the shell, liquid, frozen, and powdered form); eggs pasteurized in the shell are heated enough to kill bacteria, but not to cook the egg.
Commercial products are made using pasteurized eggs; therefore, these items are safer to consume (pregnant women should read the label to make sure and look for the word “pasteurized”.)
In the U.S., eggs should be stored in the refrigerator.
Hands, and all utensils or surfaces should be washed thoroughly after contact with raw eggs, including shells.
Eggs should be cooked until the yolks and whites are firm (and scrambled eggs are dry and firm).
Baked egg mixtures such as quiches, frittatas, and French toast egg dishes/casseroles should be cooked until the center of the mixture reaches 160° F.
Women should avoid icing, meringue, and whipped topping recipes that use raw egg whites; frostings and meringues that are made by combining hot sugar syrup with beaten egg whites are safe to eat.
Read Food Safety for more detailed information on safe food preparation.
Families who own backyard chickens, hedgehogs, or turtles should: wear gloves, use routine veterinary care, keep facilities clean, dispose of waste properly, wash hands thoroughly after contact, and follow all local ordinances regarding the ownership of poultry, specifically.
Women should also consider sharing and submitting their experience below regarding salmonella or food poisoning during pregnancy. This can help other women recognize the possible signs and course of infection as well as the need to call an HCP for potential testing and treatment.
Partners/Support
Partners and family members of pregnant women should follow the same guidelines above regarding egg safety. Any individual who cooks or prepares food should learn proper food safety and best practices to avoid foodborne illness – for the entire family.

Resources
Salmonella Fact Sheet (U.S. Centers for Disease Control and Prevention)
Current Salmonella Outbreaks (U.S. Centers for Disease Control and Prevention)
Egg Storage Chart (Foodsafety.gov)
Tips to Reduce Your Risk of Salmonella from Eggs (U.S. Centers for Disease Control and Prevention)
Consumer Information about Egg Safety (U.S. Food and Drug Administration)