Safe Food Handling

Food safety practices are not as commonplace as they should be, and millions of Americans experience foodborne illnesses every year. While most individuals will recover with only supportive management (i.e. fluids, rest), pregnant women may experience more severe illness/symptoms.
However, there is no evidence that pregnant women are more likely to contract a foodborne illness than non-pregnant individuals; but certain foodborne pathogens, when severe, can pass through the placenta and infect the fetus before delivery – presenting possible life-threatening complications.
Further, while dehydration and electrolyte imbalances are manageable in non-pregnant individuals, these complications can be more emergent during pregnancy.
Risks for these infections can be dramatically reduced through proper food-handling, storing, cooking, and eating habits. Any habit is difficult to break, but the improvement of food safety in and around the kitchen at home can help prevent illness in every member of the family.
Background
Food safety is very important during pregnancy. Although non-pregnant individuals who contract a foodborne illness usually recover in less than a week with no complications, pregnant women with foodborne illness can experience more severe complications (read Salmonella, E. coli, and Listeria).
Proper food safety practices are not easy and require a lot of time and attention, and even completely new behavior. For individuals who do not regularly practice adequate food safety, these changes may:
Take more time
Feel slightly more inconvenient
Change a preferable taste in food (cooked instead of raw, firm eggs instead of runny)
Require new behavior and attentiveness
Require new tools (thermometer, additional cutting boards)
Feel awkward at times (using a thermometer when others are cooking, asking food servers more questions, placing restrictions on/at dinner parties)
But will:
Help eliminate risk for foodborne illness in the mother, fetus and newborn, and the entire family (*foodborne illness can transfer to the fetus/newborn during pregnancy)
Help relieve anxiety and concern about possible illness
Likely become more permanent habits
Help promote the overall health of the mother and her pregnancy
Proper food hygiene and safety techniques do not have to run a household, they should complement it. Although certain methods and recommendations can feel overwhelming, good prevention techniques can be broken down simply enough to remember every day and have a strong, positive impact on health.

Foodborne Illness
Food safety and good hygienic practices are important strategies in the prevention of foodborne illnesses, in which more than 200 have been identified. Some of the most common are:
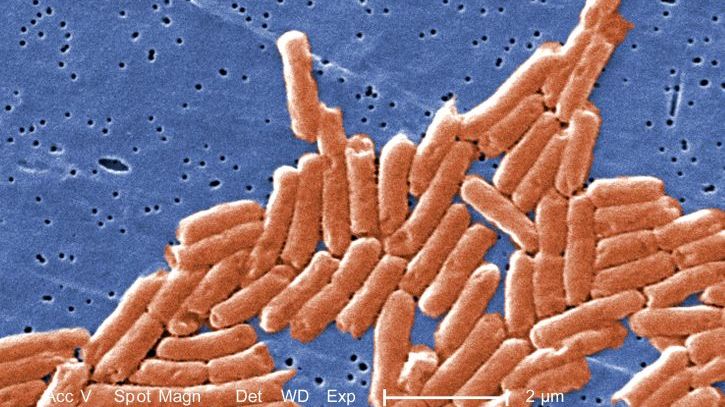
E. coli: Escherichia coli (E. coli) are a large group of bacteria found in the environment, foods, and intestines of people and animals. There are many strains, most of which do not make individuals sick. However, other strains of E. coli can cause three different types of illnesses: gastrointestinal, urinary tract infections, and neonatal meningitis. Read more.
Listeria: Listeriosis is a rare foodborne illness caused by the bacterium Listeria monocytogenes (Listeria), commonly found in soil, vegetation, and animal feces. Listeria is known to disproportionately affect immunocompromised patients, elderly people, pregnant women and newborns. Although very rare, the consequences of invasive infection in a pregnant woman can result in neonatal complications, with a high mortality rate. Read more.
Norovirus: Norovirus is a very contagious virus that produces nausea, vomiting, and diarrhea in infected individuals, and is commonly known as a “stomach bug”; this virus can also be easily transmitted through food. Norovirus can cause severe dehydration and electrolyte imbalance in pregnant women.
Salmonella: Salmonellosis is an infection caused by Salmonella bacteria; it is a kind of food poisoning caused by eating contaminated or improperly cooked food, most often from poultry and eggs. It can also occur through contact with live poultry. Severe salmonella infection has been documented to cross the placenta and infect the fetus. Read more.
At Home
Of the reported foodborne illness outbreaks reported in the United States (U.S.) between 1998 and 2008, 9% to 15% were from food-related incidents in the home, with Norovirus and Salmonella being responsible for more than a third of illnesses.
In Europe, approximately one-third of foodborne illness cases were attributed to the home, most of which were due to Salmonella.
At least two studies have reported that the kitchen is more heavily contaminated with fecal matter than bathrooms.
One of the most important ways to prevent foodborne illness in the home other than the proper storage of food itself, is to pay attention to the activities that occur in and around the kitchen; women should also be careful not to cross-contaminate or introduce bacteria to where food may be prepared and/or eaten.

One study noted how the kitchen sink is used for many activities ranging from hand washing, food rinsing, dish washing, soaking clothing, bathing small children and pets, wetting brooms and mops, and dumping food.
Kitchen counters are used for school activities, dirty clothing, backpacks and purses, old newspapers and mail, small house plants, and raw and cooked food preparation and food presentation.
All these items can transfer harmful bacteria to a surface that may contaminate prepared food which could be touched or eaten by anyone in the household.
Refrigerator and Freezer
Refrigerator temperature of 40° F (4° C) or below, and freezer to 0° F (-18° C) or lower is often recommended to prevent the growth of bacteria; bacteria can grow quickly in temperatures between 40° and 140° F (4° C to 60° C).
Refrigerators carry a lot of bacteria, and therefore have the potential to transfer bacteria to foods meant to be eaten raw (i.e. fruits/vegetables). Egg cartons can be contaminated with salmonella, as well as chicken and meat packaging. Depending on where these items are placed in the refrigerator, any item meant to be eaten raw can be placed in those same locations later, potentially contaminating the raw item.
Women should store raw produce on one side of the fridge, and eggs, chicken, meat, and fish on the other side and toward the bottom, to prevent juice/drippings from contaminating anything underneath.
Ideally, produce should be washed/chopped prior to storage in the fridge, but this is not always possible. Women/family members should just stay aware of all cross-contamination possibilities inside a refrigerator and clean the trays/shelves often.
Items stored on the door of the refrigerator may not be as cold as items toward the back.
Women should use the plastic clear bags available in the meat and egg sections of some grocery stores to pick up meat packages and egg cartons, and place them inside the bag. Since the outside of the bag is presumably free of bacteria, it can then be placed inside the refrigerator without contaminating a shelf.
Meat, poultry, eggs, seafood, dairy, and ready-to-eat foods should be refrigerated or frozen within two hours of purchase; leftovers should not be left out for more than one to two hours, depending on the room temperature. Note: This does not mean that at 2 hours and 10 minutes the product is necessarily bad; but bacteria likely starts to grow about or before that time.
Sliced fruits and vegetables should always be kept in the refrigerator (i.e. fruit salad), and not left out on a counter (solid fruit is fine).

Women should check the refrigerator often for sell-by and use-by dates, especially meat, eggs, and dairy.
It is a general rule that unopened packages may last about 2 weeks in a refrigerator, and opened containers of food about 3 to 5 days; some products have lengthy expiration dates that quickly change to only days once the product has been opened (check label).
For example, a product may have: Expiration date: 12 27 2020; but also: Use within 3 days after opening.
Defrost/Thaw
Freezing stops the growth of bacteria which is why frozen items can keep for months at a time. However, once that item starts to thaw, any bacteria present will begin to grow.
Women should defrost raw meat, poultry, fish and seafood in the refrigerator whenever possible. Depending on the size of the protein, this could take more than 24 hours. It is not recommended to thaw food on a counter at room temperature.
Food can also be thawed in a sealed bag in cold water (such as frozen shrimp/chicken breasts) or in the microwave using the “defrost/thaw” option by weight. If the microwave is used, the food item should be cooked immediately afterward.
Large whole chickens and turkeys are traditionally thawed in their current packaging in sinks or bathtubs in cold water that is changed every 30 minutes. Full thawing may take about 30 minutes per pound. However, the U.S. Department of Agriculture recommends the refrigerator whenever possible, allowing for one full day for every 4 to 5 pounds. The tub/sink needs to be cleaned afterward due to possible salmonella on the chicken/turkey packaging.
A thawed chicken or turkey can remain in the refrigerator for an additional 1 to 2 days. The purchase of a refrigerated turkey/chicken can help women avoid the thawing step, but it cannot be purchased very far in advance.
Note: It is perfectly safe to cook a frozen or partially frozen turkey/chicken, it will just take longer (always use a meat thermometer).
Women should not refreeze any food item that has already been thawed. Any leftovers need to be thrown away.
Food Preparation
Food preparation is a major point of possible cross-contamination that can be prevented with a few techniques that are easy to remember.
The best line of action for any food preparation is to have awareness of what is happening and where; keep raw food and raw meat away from finished, prepared food, to include all dishes, cutting boards, utensils, and cookware.
The best starting recommendation is to use distinct cutting boards/knives:
One cutting board/knife for raw meat
One cutting board/knife for raw foods (vegetables, etc.)
However, one of each can be used if the produce is cut first. The produce can then be placed on a separate dish, then the meat can be cut using the same cutting board and knife. The board and knife need to be immediately cleaned or placed in a dishwasher to avoid mixing them up later, and hands need to also be washed before touching anything else.

Hand washing: hands need to be washed anytime unrinsed produce and raw meat has been handled, and after each different type; it is important not to touch raw meat and then touch produce – even produce that will eventually be cooked. Although cooking will kill that bacteria, doing it this way each time helps build up the habit and lessens the possibility for mistakes.
Hand washing is the cornerstone of all infection control.
Hands should be washed thoroughly for at least 20 seconds with warm, soapy water, including in between fingers, under nails, and over the nail beds. Gentle friction is key to removing as much bacteria/viral organisms as possible.
It is important the faucet is not touched with contaminated hands (raw chicken) and touched again after washing, or the process needs to start over.
In general, when preparing food, hands need to be washed after using the bathroom, touching raw/uncooked/unwashed food items, touching contaminated utensils, and after touching a cell phone or tablet.
Disposable gloves can also be used when handling chicken; gloves need to be removed inside out after handling. Women should be careful not to get raw meat on their wrists or any part of their arms not covered, or juices inside the gloves.
Chicken does not need to be rinsed prior to cooking; this is not based on evidence; anything seen as undesirable on the chicken should be cut away. Further, cooking will remove anything harmful on the chicken. Rinsing chicken spreads salmonella throughout the kitchen sink, which can easily transfer to other foods.
However, produce should always be rinsed under cold water.
Soaking produce using vinegar, lemon, or a “vegetable soap” has not been shown to be more effective than cold water alone, and could introduce additional chemicals.
While research is still attempting to determine the best method for sanitizing fresh produce, to date, the best method appears to be rinsing with cold water – without special rinses, solutions, soaps, or chemicals.

Notably, the same study also indicated that pre-washed and ready-to-eat lettuce was still contaminated with a significant amount of bacteria and should still always be washed by the consumer.
A study that evaluated the rinsing of lettuce leaves showed a significant reduction in bacteria after running the leaves under a high flow rate of cold water from a faucet. Simply rinsing/soaking lettuce leaves in a bowl or using a low flow rate was not nearly as effective.
Although higher flow water does “flatten” the texture of some different types of leaves, it is effective (romaine lettuce holds its shape well). A salad spinner can be effective at drying leaves and improving their shape/texture after rinsing.
Cooking/Baking/Grilling
When food preparation is complete and ready for cooking, the key preventative technique remains the same – use one plate for raw meat and one plate for cooked meat, to include utensil use and serving ware (spatula, etc.).
This includes marinades, especially when grilling; if a grill brush is used to marinade raw meat, that same container of marinade and brush cannot be used to marinate finished meat. The marinade can be used on finished meat only if boiled first.

Vegetables and raw meat can be cooked together if the meat has been thoroughly cooked and the juices run clear.
When using a microwave oven, the turn table is there to rotate food and provide more even cooking. If a turntable is not available, food should be covered by another microwave safe plate or bowl and repeatedly stirred and turned throughout cooking.
Doughs and batters, to include for desserts, muffins, and breads, should not be eaten or tasted raw, even without raw eggs – flour can also be contaminated with bacteria.
According to a CDC report published in April 2021, flour is increasingly recognized as a cause of STEC (E. coli) outbreaks. Raw flour is not a ready-to-eat product and infection can occur through consumption of raw doughs and batters.
For example, raw flour was the cause of an outbreak from 2018 to 2019 in which twenty-one cases were reported from nine states. The majority of individuals reported eating, licking, or tasting raw homemade dough or batter prior to illness onset.
Cooking Temperature
Cooking food to the proper temperature is a primary factor in preventing foodborne illness. A thermometer should be used for all protein (including egg) and baked dishes, including breads, desserts, quiches, hamburgers, hot dogs, steak, fish, and chicken.
A food thermometer should always be placed in the thickest part of the dish, which takes the longest time to cook. It is possible – and common – for other parts of a dish to reach the correct temperature prior to other parts. Some sources indicate the thigh is the best place for poultry, while others indicate the thickest part of the breast is the best location (check both). It is important to avoid bone or fat, which can skew the temperature result.
Color of food is not a reliable indicator of safety or doneness.
Recommended temperatures:
Fish/Seafood: 145° F
Read more detail regarding eating fish and seafood during pregnancy here.
Beef, veal, lamb steaks and roasts: 145° F then let rest for 3 minutes (previously recommended at 160° F/*updated in May 2011)
Pork chops, ribs, and roasts: 145° F then let rest for 3 minutes (changed in May 2011)
Egg Dishes: 160° F; in general, cook eggs until hard and firm
Read more detail regarding egg handling, storing, and safety here.
Ground beef, pork, veal, and lamb: 160° F
Note: All ground beef and hamburger should be cooked until completely brown AND the temperature reaches 165° F. The center should not be pink, and just because the center is brown, does not mean it is fully cooked.

At least one study determined that ground beef can appear brown in color (or turn brown prematurely) well before the internal temperature reaches 165° F. This was theorized to occur more often in frozen beef that was thawed overnight in a refrigerator. The study also noted that juice color and texture were also not good indicators of doneness.
Ground turkey and chicken: 165° F
Casseroles and stuffings: 165° F
Poultry (including whole and parts of chicken and turkey): 165° F

Hot dogs, luncheon meats, and deli meats: reheated to steaming hot or 165° F
Hot dogs should never be eaten straight out of the package, even if the package indicates they are full cooked; hot dogs should be cooked/reheated until steaming hot.
Reheat fully cooked hams packaged at a USDA-inspected plant to 140° F.
For fully cooked ham that has been repackaged in any other location or for leftover fully cooked ham, the recommendation is to heat to 165° F.
Leftover food meant to be warm: reheat to 165° F
A wired/wireless thermometer can be purchased at most grocery stores that allows the thermometer to stay inside while the oven door is closed and the gauge remains on the outside. This avoids the constant need to open the oven door, releasing warm air, to check the temperature.
Leftovers
Leftovers need to be placed in the refrigerator with one to two hours at room temperature (sooner in warmer weather/picnics) and consumed within two to three days. Leftovers should only be reheated once, so only the individual portion meant to be eaten should be reheated.
Opened aluminum cans should never be placed in the refrigerator. If only some of the inside contents of an aluminum can are used, the rest should be placed into a plastic or glass container and placed into the refrigerator.
If leftovers are placed in a refrigerator while still warm, placing the food in shallow containers can cool the food down quicker so the food does not change the temperature of the refrigerator, even temporarily.
All leftover meat should be reheated to 165° F, and all sauces, soups and gravies should be brought to a boil.
Cleaning
Dishes need to be washed with warm/hot soapy water, preferably with a scrub brush instead of a rag, cloth, or sponge. Dishes should not be submerged in a sink full of water for cleaning.
Food thermometers also need to be cleaned in warm, soapy water between each temperature reading, per the manufacturer’s instructions.
Clean sinks, kitchen surfaces, or containers immediately after they have been in contact with raw meat. Disinfecting wipes/sprays can kill most bacteria and viruses on surfaces (check labels).

Although disinfectant wipes contain chemicals in concentrations of 0.01% to 0.1%, this concentration is high enough to break apart bacterial cells, but not human skin. Disinfectant wipes are designed to be used by a bare hand, and systemic absorption is therefore expected to be very minimal.
If pregnant women are still concerned, they can wear a disposable glove when handling disinfectant wipes or place a paper towel over the wipe to avoid absorption through the hand as much as possible. Washing hands immediately after use may also prevent absorption but this has not been studied. Women should also read the manufacturer’s instructions on the label for proper use.
Paper towels should be used when possible, but to reduce waste, hand towels can be designated solely to dry wet, clean hands. Any dish towels used should be cleaned everyday in the hot wash cycle of a washing machine.
Workplace
Many workers eat lunch at their desks, which can pose a foodborne illness risk if not cleaned properly. One study reported that most individuals rarely or never clean their workspace.
Many women use reusable lunch boxes/bags to take to work. Women should include enough ice packs to keep their lunch cold if a refrigerator is not available. The inside and outside of lunch boxes/bags should be wiped down and air dried with a disinfectant wipe daily – preferably in the evening to let it air out overnight.
Women can also carry “to go” packs of disinfectant wipes to clean a shared workspace or break area prior to eating lunch.
If leftovers were packed, women should make sure to reheat them in an office microwave until evenly reheated and steaming hot (or food thermometer, if available, reaches 165° F).
Women should not use office cleaning supplies (sponges, scrub brushes) unless they know the last time they were cleaned or replaced.
Social Events
Attending social events in which food will be available can be unnerving for some pregnant women when attempting to choose what to eat without concern. It is not always possible to know how all foods are prepared or even who made it, depending on the event.
For those who may get very anxious about eating food they did not prepare, those women should eat what they can from home prior to attending the event or bring their own food if and when possible.
Women should also not be afraid to ask about certain foods or how they were prepared.

If women attend an event, and do not know how long the food has been out, they may want to skip certain foods or ask the host. In general, foods should not be outside for more than one hour before being placed into a refrigerator, no matter whether the food is supposed to be hot or cold. Foods at room temperature may be safe for up to two hours before bacteria starts to grow.
Dining/Take Out
Women should ask the server any questions they have about anything on the menu, how the food is prepared, and what ingredients may be included. They also should not be afraid to request substitutions if accepted by the restaurant.
Women can ask their server if raw eggs or unpasteurized dairy are used (especially in certain desserts), and request that all ground beef is well done and fully cooked and brown throughout.
Although very rare, deli meat can carry listeria, and most restaurants do not heat their luncheon meat for sandwiches until steaming hot. It is up to each individual woman whether she wants to eat deli meat (that has not been reheated) during pregnancy (read Listeria).
Grocery Shopping
Improved standards and surveillance techniques have reduced the prevalence of contaminated foods at grocery stores, although it still occurs – especially in ready-to-eat foods and some raw produce, such as lettuce.
However, reusable grocery bags, a growing trend for the environment, can cause foodborne illness if they are not regularly cleaned, especially if they are used for things other than groceries. One study found large numbers of bacteria (including fecal bacteria) in every reusable bag collected from shoppers outside a grocery store (compared to none in traditional plastic bags or brand-new reusable bags).
Pregnant women should avoid carrying raw meat, seafood, poultry, and egg cartons either in the reusable bags completely, or keep them separated from the bags used to carry other food products. These bags can be separately marked to be cleaned (although all the bags should undergo regular washing).

General tips for food safety during grocery shopping include:
Wiping down the cart, handles, or basket with disinfecting wipes
Using small plastic bags to place over raw meat, seafood, pork, and poultry containers before placing into the cart
Buying cold and frozen items near the end of the trip; if the outing includes additional stops after the grocery store, women can pack a cooler with ice if they will not get home within an hour or two
Checking fruits and vegetables to look for mold, small bugs, cuts (from equipment), bruises, and general damage
Refrigerating or freezing cold or frozen foods immediately upon returning home
Buying pasteurized juice and egg, cheese, milk, and other dairy products
Pay attention to all sell-by, best if used by (or before), and use-by dates on all foods purchased.
Action
The risk of foodborne illness during pregnancy can be dramatically reduced through proper food-handling, storing, cooking, and eating habits. Any habit is difficult to break, but the improvement of food safety in and around the kitchen at home can help prevent illness in every member of the family.
Women should follow the guidance above, and direct any questions they have regarding food safety during pregnancy to their health care provider (HCP).
Women should also read more information on salmonella, listeria, E. coli, and diarrhea to learn signs and symptoms of possible foodborne illness.
Partners/Support
Partners and family members of pregnant women should read and follow the same guidelines above regarding food safety. Any individual who cooks or prepares food should learn proper food safety and best practices to avoid foodborne illness – for the entire family.
Resources
Cold Food Storage Chart (Food Safety.gov)
Food Safety for Pregnant Women (U.S. Food and Drug Administration)
Safe Food Handling for Pregnant Women (Healthy Canadians)
Consumer Information about Egg Safety (U.S. Food and Drug Administration)
Food Safety Tips for the Holidays (U.S. Centers for Disease Control and Prevention)
Turkey Basics: Safe Thawing (U.S. Department of Agriculture)
Food Safety in a Disaster or Emergency (FoodSafety.gov)