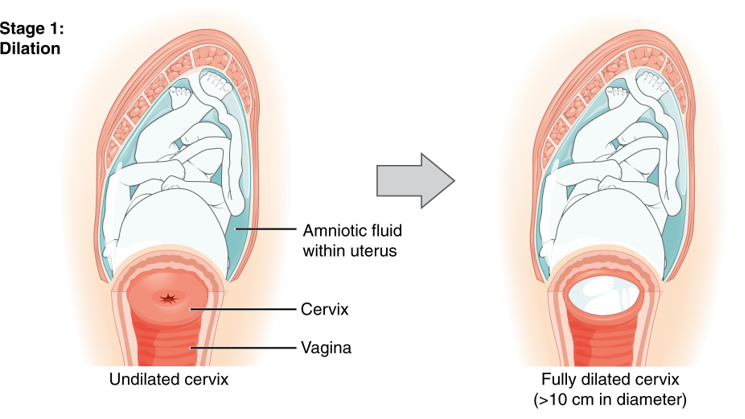
Dilation and Effacement

Dilation (10 centimeters) and effacement (100%) must occur before the baby can pass through the cervix and vagina for delivery. However, this process cannot take place until cervical ripening occurs – which can start hours, days, or weeks before labor.
After ripening, dilation and effacement will occur simultaneously, but effacement usually completes first. As the cervix effaces, this causes the expulsion of the mucus plug.
With the progression of contractions and the fetal head pressing down onto the cervix, the cervix completes dilation and effacement, and women can begin pushing (second stage of labor).
Under the definition of active management of labor, women should dilate approximately 1 cm/hour. However, research conducted after this definition was established indicates women – especially those in a first delivery – can dilate much slower than this expected rate and still be experiencing normal labor.
Therefore, as long as fetal heath assessment is reassuring, women should be allowed to take the time they need to fully dilate, which can help avoid unnecessary augmentation/delivery methods (oxytocin, amniotomy, assisted delivery, or cesarean section).
Background
Prior to vaginal delivery, the cervix must be 100% effaced and 10 centimeters (cm) dilated (efface = thinning; dilation = opening). This is the amount of dilation necessary for a fetal head to pass through the cervix and into the vaginal canal.
Cervical ripening is a step prior to dilation and effacement in which the cervix begins to soften in preparation for labor. Ripening can begin weeks or days before labor. Near term, the body makes natural prostaglandins which aid in the breakdown of cervical collagen. Pharmaceutical prostaglandins are often used prior to the induction of labor to safely and effectively ripen the cervix in women whose cervix did not ripen on its own.
Once the cervix ripens, it is ready to respond to contractions. Contractions put pressure on the softened cervix, which causes it to efface and dilate; contractions also force the presenting part of the baby (usually the head) down onto the internal os of the cervix (part of the cervix touching the baby's head), which also helps the cervix dilate.
Effacement
Effacement, which begins at the internal os, reflects the length of the cervical canal compared with that of an uneffaced cervix. When it is reduced by one-half of its prior length, it is considered 50% effaced. When the cervix becomes as thin as the part of the uterus surrounding it, it is considered completely (100%) effaced. At 100% effaced, the cervical length transforms from about 3 cm to a circular cavity with paper-thin edges.
As the cervix shortens, it causes the expulsion of the mucus plug.
Dilation
Dilation is determined by estimating the average diameter of the cervical opening by sweeping the finger from one side of the cervical opening to the other side.
The internal os dilates first, and the external os – the part of the cervix facing out toward the vagina – does not feel enough of this same pressure until effacement has progressed.
Once effacement has progressed, contractions cause a centrifugal pull on the lower part of the uterus and cervix, which forces the the cervix to open. Ten centimeters is considered fully dilated as a baby's head can pass through a cervix at this diameter.
Women are advised to avoid pushing until 10 cm is reached, even though the urge to do so may be very powerful between 8 and 10 cm (also known as the "transition" stage). Although evidence regarding "pushing prior to full dilation” is very limited, it could cause the mother to become too tired, as the baby will likely make no progression downward through it (whether pushing too early causes cervical trauma is debated).
Dilation Rates
Cervical dilation rate is highly individualized and is affected by several variables. There is no definitive minimum amount of time during labor in which all women are expected to fully dilate.
During labor, and after admittance to a hospital/birthing center, the HCP will monitor the progress of labor by periodically evaluating the cervix for dilation and effacement, as well as the baby's position and location.
The rate of cervical dilation (cm/hr) in the first stage of labor (to full dilation) usually forms the basis of decision-making by the HCP as to how delivery will ensue. For example, an HCP may determine that dilation is too slow, and may recommend augmenting labor through oxytocin or amniotomy – which is a common practice called active management of labor.
Active management includes taking purposeful steps to speed up labor, even if there is technically no medical reason to do so. However, some women may prefer this method.
Therefore, in the absence of fetal distress, it is the woman's decision whether she wants an HCP to utilize methods to speed up her labor.
Under active management, the slowest acceptable rate of dilation is defined as 1 cm/hr. However, it is currently assessed that 1 cm/hr, especially in first deliveries, may be unrealistically fast.
This higher expectation of cervical dilation during active labor is linked to diagnoses of labor dystocia ("failure to progress") defined by the American College of Obstetricians and Gynecologists (ACOG) as “slow, abnormal progression of labor".
Over diagnosis of dystocia can lead to unnecessary interventions, especially cesarean section; this is critical, as some women may need a cesarean section for every subsequent delivery thereafter. Cesarean section also carries more risks than vaginal delivery.
Although some women may dilate at 1 cm/hr or faster, studies indicate that most women during their first delivery dilate less than 1 cm/hr. The established rate of 1 cm/hr under the active labor definition was determined prior to this kind of research.
Additionally, progress may be slow between 4 and 6 cm, but accelerates thereafter. If active labor is kept at a definition of 4 cm rather than 6 cm, this would also lead to a potential false diagnosis of slow labor.
The founder of active management wrote himself that “…the majority of patients are in active-phase labor by the time the cervix reaches 4 cm, but many are not".
On average, the active phase of labor (defined as 4 to 10 cm) may last 5 to 7 hours in a first delivery, and 2 to 4 hours in a subsequent delivery.
However, as stated above, active labor may not truly start in some women until 6 cm. The concern with expected dilation rates is that women may be diagnosed believed to be in active labor at 4 cm (but are not), and then held to the rate of 1 cm/hr which they will not reach – and therefore, may have unnecessary augmentation interventions.
The latent phase (1 to 4 cm) is difficult to time and duration varies but it is estimated to average about 8 hours in first time deliveries, and 5 hours in subsequent pregnancies. Duration is considered abnormal if this stage lasts more than 20 hours and 12 hours, respectively.
A more realistic rate of dilation needs to be established so that proper interventions can take place, when needed. The slower end of normal may be closer to 0.5 cm/hr in earlier active labor, while it accelerates as labor progresses. It is further assessed this rate is achievable by 80% to 90% of women.
Further, one study found that some women had no perceivable change in dilatation for more than 2 hours during the period before 7 cm dilation.
However, regardless of dilation rate prior to 7 cm, it is well established that dilation rates progressively accelerate from 7 or 8 cm to 10 cm.
Action
Women should ask their HCP what their dilation expectation rate is, and how the facility staff handles "slower" progression of labor.
Women should also learn about augmentation methods of labor, in the event they may be needed (fetal distress). Some women may even prefer to have their labor augmented.
Since most discussion regarding dilation rates and possible interventions occurs during labor, doulas can assist in this regard. Doulas can help communicate information, and serve as intermediaries, between the HCP and the pregnant woman/couple.
Resources
Interactive Tool - Cervical Dilation and Effacement (St. Luke's Hospital, Chesterfield, MO)
Video (1:21 seconds) explaining how an HCP examines the cervix of a pregnant woman.